Ketamine-Assisted Psychotherapy: Cutting-Edge Research Insights
Why Ketamine-Assisted Psychotherapy Research is Changing Mental Health Treatment

Ketamine assisted psychotherapy research shows remarkable promise for people who haven't found relief through traditional treatments. Recent studies reveal that combining ketamine with therapy can help 86% of PTSD patients no longer meet diagnostic criteria, while achieving 65.8% abstinence rates in alcohol addiction at one-year follow-up.
Key Research Findings:
- 91% improvement in generalized anxiety among healthcare providers with PTSD
- 79% improvement in depression scores across multiple studies
- Sustained benefits lasting 3-6 months when therapy is integrated
- Treatment-resistant conditions showing significant response rates
- Multiple psychiatric disorders benefiting from combined approach
The research consistently shows that adding psychotherapy to ketamine treatment produces better outcomes than ketamine infusions alone. While ketamine infusions typically show relapse within 18 days, ketamine-assisted psychotherapy (KAP) extends benefits for months.
Study populations include:
- Treatment-resistant depression
- PTSD and complex trauma
- Substance use disorders
- Chronic anxiety and panic
- Eating disorders
As someone who has spent decades working with trauma survivors and exploring innovative therapeutic approaches, I've closely followed ketamine assisted psychotherapy research developments. My experience with intensive therapy models and trauma-informed care has shown me how breakthrough treatments can offer hope when traditional methods fall short.

KAP 101: Differentiating Ketamine-Assisted Psychotherapy from Ketamine Infusion Clinics
If you're exploring ketamine treatment options, you've probably noticed two very different approaches: ketamine-assisted psychotherapy (KAP) and ketamine infusion clinics. While both use the same medication, they're as different as a home-cooked meal and fast food—same ingredients, completely different experience and results.
Ketamine made its debut in 1962 as a dissociative anesthetic for surgery. Sixty years later, this anesthetic has split into two distinct mental health pathways. Traditional infusion clinics borrowed the medical model—you sit in a chair, get an IV, and hope the medication does its magic. It's straightforward, clinical, and treats ketamine like any other psychiatric drug.
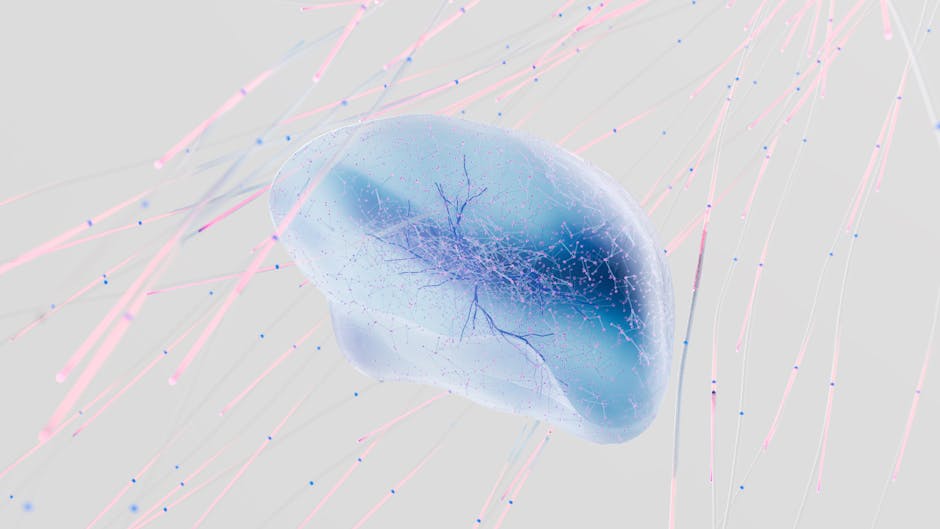
Ketamine-assisted psychotherapy research tells a different story. This approach sees ketamine not as a cure, but as a powerful tool that opens doors in your mind. If your brain is a house that's been locked up tight, ketamine helps find the keys. But you still need someone skilled to help you walk through those doors and make sense of what you find inside.
The magic happens during what scientists call the neuroplastic window—a period starting within hours of your ketamine session when your brain becomes incredibly flexible and ready to form new connections. This window can stay open for several days, creating an amazing opportunity for real therapeutic work. Miss this window, and you've missed the point entirely.
Set and setting aren't just fancy terms—they're game-changers. Your mindset going into the experience and the environment around you shape everything that happens. Research shows that people sometimes feel abandoned in IV infusion settings, sent home while still under the influence without proper support.
The multidisciplinary team approach sets KAP apart. While infusion clinics typically involve only medical staff checking your vitals, KAP brings together trained psychotherapists, medical professionals, and sometimes additional specialists working together to ensure you're not just safe, but actually healing.
Psychotherapy integration happens before, during, and after your ketamine sessions. Your therapist helps you prepare mentally and emotionally, stays with you during the experience, and then works with you afterward to make sense of insights and integrate them into daily life. This isn't just nice-to-have support—it's what makes the difference between temporary relief and lasting change.
| Aspect | KAP | Infusion Clinics |
|---|---|---|
| Dosing Route | IM, sublingual, oral | Primarily IV |
| Therapeutic Support | Extensive prep & integration | Minimal |
| Setting | Therapy-focused environment | Medical clinic |
| Team | Therapist + medical | Medical only |
| Follow-up | Structured integration sessions | Limited |
| Duration of Care | Weeks to months | Days to weeks |
Why Context Matters
The therapeutic alliance—that special bond between you and your therapist—isn't just relationship building. Ketamine assisted psychotherapy research from MDMA and psilocybin studies shows that stronger therapeutic relationships directly predict better outcomes. When you trust your guide, you're more willing to explore difficult territory.
Your environment matters more than you might think. Soft lighting, carefully chosen music, and thoughtful decor aren't about creating a spa experience—they're about safety and healing. When you're in a vulnerable, introspective state that ketamine can create, these environment cues help your nervous system stay calm and open to change.
The neuroplastic window represents the heart of why KAP works so well. Ketamine boosts Brain-Derived Neurotrophic Factor (BDNF)—think of it as fertilizer for your brain. Your neurons become more willing to grow new connections and let go of old, stuck patterns. But without skilled therapeutic work during this window, you might miss the chance for lasting change.
State of the Science: Ketamine Assisted Psychotherapy Research in 2024
The world of ketamine assisted psychotherapy research has exploded in 2024, painting an exciting picture across multiple mental health conditions. What started as studies focused mainly on depression has grown into a rich landscape of research covering everything from PTSD to eating disorders.
Treatment-resistant depression remains the heavyweight champion of ketamine research—and for good reason. When the FDA approved ketamine for this condition in 2019, it opened the floodgates for more comprehensive studies. But researchers didn't stop there. They've been busy exploring how ketamine can help with PTSD, substance use disorders, anxiety spectrum conditions, and even eating disorders.
One of the most fascinating developments is the emergence of group therapy formats alongside traditional individual sessions. A cohort study involving 94 healthcare providers showed remarkable results using a group-based community approach. This is huge news for accessibility—group sessions could help more people access this life-changing treatment.
The numbers speak for themselves: a systematic review of 19 studies involving 1,008 patients found largely positive outcomes across the board. What makes this even more impressive is the diversity of conditions being treated successfully.
Key Findings from Ketamine Assisted Psychotherapy Research on Depression & PTSD
Here's where the research gets really exciting. A 2019 study tracking 235 patients found something that challenges everything we thought we knew about treating severe mental health conditions. The participants with complex PTSD or developmental trauma actually showed the highest levels of improvement on their Beck Depression Inventory scores.
Think about that for a moment. The people with the most complex, deep-rooted trauma—the ones who've often been told they're "treatment-resistant"—were the ones who improved the most. It's like finding that the mountain everyone thought was impossible to climb actually has a hidden path to the summit.
For PTSD specifically, the results are nothing short of remarkable. In a 2022 study, 86% of participants who had PTSD at the beginning no longer met the diagnostic criteria after completing their ketamine-assisted therapy program. To put this in perspective, traditional PTSD treatments typically see much lower remission rates.
The durability question—how long do these improvements last—reveals why therapy integration matters so much. While ketamine infusions alone show people typically relapse within just 18 days, ketamine assisted psychotherapy research demonstrates sustained improvements lasting 12 weeks or longer. A large study of 1,806 adults found strong effect sizes maintained at six months, proving that the combination approach creates lasting change.
Relapse Prevention: Insights from Ketamine Assisted Psychotherapy Research on Addiction & Suicidality
If the depression and PTSD results impressed you, wait until you see what happens with addiction treatment. This is where the difference between ketamine alone and ketamine with therapy becomes crystal clear.
Alcohol use disorder research shows results that would make any addiction specialist do a double-take. In a randomized controlled trial, 65.8% of people getting ketamine plus psychotherapy were still abstinent at the one-year mark. Compare that to just 24.0% in the standard treatment group. That's nearly three times better—the kind of improvement that changes lives and families.
Cocaine dependence studies are equally impressive. Researchers combined ketamine with mindfulness-based relapse prevention and found 48.2% cocaine abstinence compared to only 10.7% with a control medication plus the same therapy. The ketamine group had 5.7 times higher odds of staying clean.
Suicidal ideation research is still developing specifically for KAP, but the broader ketamine studies show rapid drops in suicidal thoughts. The research on neuroplastic window suggests that integrating psychotherapy during this critical period helps people build lasting tools for managing future crises and addressing the root causes of their suicidal thinking.
What makes these addiction and suicidality findings so powerful is that they represent hope for conditions that have historically been very difficult to treat long-term. The combination of ketamine's neuroplastic effects with skilled therapeutic intervention appears to create a window for deep, lasting change.
How Psychotherapy Improves Ketamine: Mechanisms & Modalities
The magic of ketamine assisted psychotherapy research lies in understanding how a medication and therapy work together in ways that neither can achieve alone. Think of ketamine as opening a window in your brain—but without skilled therapy to guide what happens during that opening, the opportunity for healing might slip away.
When ketamine enters your system, it blocks what scientists call NMDA receptors. This triggers a fascinating chain reaction: your brain releases more glutamate (a key chemical messenger), and production of brain-derived neurotrophic factor (BDNF) shoots up. BDNF acts like fertilizer for your brain, helping neurons grow new connections and pathways.
This creates what researchers call the "neuroplastic window"—a period when your brain becomes remarkably adaptable and ready to learn new patterns. But here's the crucial part: this increased flexibility needs direction. Without therapy to guide the process, it's like having a perfectly tuned instrument with no one to play it.
Memory reconsolidation offers another piece of the puzzle. Ketamine appears to make difficult memories—trauma, addiction patterns, depression cycles—temporarily "editable." During therapy sessions, these previously stuck memories can be updated with new, healthier information. It's as if you can rewrite parts of your story while your brain is in this more flexible state.

Neurobiological & Psychological Synergy
The beautiful thing about combining ketamine with therapy is how the biological and psychological effects amplify each other. Ketamine's dissociative effects can temporarily lower your psychological defenses—those protective walls we build around painful experiences. This makes difficult emotions and memories more accessible for therapeutic work.
At the same time, having a skilled therapist present ensures this vulnerable state leads to healing rather than overwhelm. The therapist acts as both guide and safety net, helping you steer insights that might feel too intense to process alone.
Psychological flexibility—your ability to adapt your thinking and behavior when life throws curveballs—seems to get a significant boost during ketamine sessions. Clients often report feeling less stuck in negative thought loops and more open to new perspectives. This increased mental agility, combined with reduced rumination, creates ideal conditions for therapeutic breakthroughs.
The meaning-making process also appears improved under ketamine's influence. Many people describe profound insights and "aha moments" that might take months to reach in traditional therapy. The integration work that follows these sessions helps transform these insights into lasting changes in how you think, feel, and behave.
Modalities Most Studied
Cognitive Behavioral Therapy (CBT) has been the most thoroughly researched approach in ketamine work. Multiple studies show that CBT following ketamine sessions produces much better long-term results than ketamine alone. One study found 66.7% response rates when six ketamine sessions were paired with ongoing CBT—particularly impressive for depression treatment.
Mindfulness-based approaches have shown remarkable success, especially for addiction. Mindfulness-Based Relapse Prevention (MBRP) teaches you to notice cravings and triggers without automatically reacting to them. This skill seems to develop more easily during ketamine's dissociative state, when you can observe your thoughts and feelings with less emotional charge.
Motivational Improvement Therapy (MET) helps people explore mixed feelings about change—that internal tug-of-war between wanting things to be different and fearing what change might bring. Combined with ketamine, this approach has shown impressive results in alcohol addiction treatment.
Exposure therapies for trauma, including prolonged exposure and TIMBER (Trauma Interventions using Mindfulness Based Extinction and Reconsolidation), take advantage of ketamine's ability to reduce fear responses. This allows people to process traumatic memories with less overwhelming anxiety.
Group circles and community-of-practice models represent an exciting development in the field. These approaches combine peer support with professional guidance, and the research suggests they can be just as effective as individual therapy while being more accessible to more people.
Protocols, Set & Setting, and Safety Considerations
When I review ketamine assisted psychotherapy research, one thing becomes clear: the details matter enormously. How ketamine is given, where it's given, and who's present can make the difference between a transformative experience and a missed opportunity.
Most research studies use intramuscular (IM) or intravenous (IV) administration, though sublingual and oral routes are becoming more popular. The typical dose ranges from 0.5-1.0 mg/kg for IM injections, with most protocols involving 3-6 medicine sessions spread over several weeks.
Successful studies include multiple preparatory meetings before the first ketamine session, followed by structured integration therapy afterward. This isn't just good practice—it appears essential for lasting results.
The medical screening process is thorough but reasonable. Studies typically exclude people with active psychosis, severe heart disease, uncontrolled high blood pressure, or active substance use (except when treating addiction specifically). Medical monitoring during sessions includes blood pressure, heart rate, and oxygen levels.
The holistic paradigm that guides effective KAP represents a shift from traditional medical thinking. Instead of just targeting symptoms, this approach considers the whole person—their mind, body, relationships, and sense of meaning.
Creating Optimal Therapeutic Containers
The research consistently shows that environment matters significantly. Participants report better experiences in spaces designed for comfort and introspection rather than medical efficiency. Think soft lighting instead of fluorescents, comfortable seating instead of hospital beds, and carefully chosen music instead of clinical silence.
Licensed clinicians trained specifically in ketamine effects and trauma-informed care are absolutely essential. The therapist's role extends beyond traditional therapy—they're preparing clients for altered states, providing guidance during potentially intense experiences, and helping integrate insights afterward.
Harm reduction principles guide every aspect of ethical KAP practice. This means starting with lower doses to see how someone responds, having medical support immediately available, and ensuring clients have safe transportation home.

Safety & Ethics
Blood pressure spikes are the most common side effect during ketamine sessions, typically resolving within 30-60 minutes. Research settings always have monitoring equipment and clear protocols for managing high blood pressure episodes.
Managing dissociation requires real clinical skill. While some dissociative effects can be therapeutic—helping people step outside their usual patterns—too much dissociation can feel frightening. Skilled therapists learn to recognize different levels of dissociation and respond appropriately.
Informed consent becomes more complex with KAP than traditional therapy. Clients need to understand both the potential benefits and risks of ketamine, what it feels like to be in altered states, and that this treatment is still relatively new.
Trauma-informed care principles become especially important because ketamine can make traumatic memories more accessible. Therapists must be skilled at recognizing trauma responses and creating safety for clients who might become emotionally overwhelmed during sessions.
Durability, Limitations, and Future Directions
The durability question might be the most important finding in ketamine assisted psychotherapy research. When you look at the numbers, the difference between ketamine alone and ketamine with therapy is striking—and honestly, it's what convinced me that this combined approach is the future of ketamine treatment.
Here's what the research shows: ketamine infusions by themselves have a median relapse time of just 18 days for treatment-resistant depression. That's barely two and a half weeks. But when you add structured psychotherapy to the mix, everything changes.
The largest study we have—involving 1,806 adults—found that people maintained significant improvements at six months. We're talking about effect sizes of 0.61-0.73, which means 48-70% of participants were still doing meaningfully better half a year later. That's not just statistically significant; it's life-changing.
But let's be honest about the limitations too. Most ketamine assisted psychotherapy research studies are still relatively small. We're talking about studies with 50-100 people, not the thousands we'd ideally want to see. This makes it harder to know exactly who will benefit most from treatment.
There's also what researchers call the "blinding problem." It's pretty much impossible to create a convincing fake ketamine experience—people know when they're dissociating. This makes it challenging to design the gold-standard double-blind studies that we rely on in medical research.
The search for biomarkers—biological signs that could predict who will respond best to treatment—is ongoing. Scientists are looking at everything from genetic markers to brain imaging patterns to blood tests. The goal is to eventually personalize treatment so we can better predict who will benefit most.
One exciting development is the emergence of digital CBT boosters and smartphone apps designed to support integration work between sessions. These tools could help people maintain their therapeutic gains over longer periods, extending the benefits even further.

Research Gaps & Needed Studies
While the current research is promising, there are some significant gaps that need filling. The biggest need is for large-scale randomized controlled trials. Most current studies involve fewer than 100 people, which limits how confidently we can apply the findings to broader populations.
We also need head-to-head comparisons of different therapy approaches. Right now, we know that adding therapy to ketamine works better than ketamine alone, but we don't know if CBT works better than mindfulness-based approaches, or if trauma-focused therapy beats general psychotherapy for specific conditions.
Long-term outcome studies extending beyond one year are crucial. The current research typically follows people for just a few months after treatment. We need to understand what happens at two years, five years, and beyond to truly assess the lasting impact of these interventions.
Diverse populations are significantly underrepresented in current research. Most study participants are white, educated, and financially stable. We desperately need research that includes people from different racial, ethnic, and socioeconomic backgrounds to ensure these treatments work across all communities.
Finally, we need more mechanistic studies—research that helps us understand exactly how psychotherapy and ketamine work together at the brain level. Understanding these mechanisms could help us optimize protocols and develop even more effective treatments.
The pipeline of upcoming trials is encouraging, with several large-scale studies planned over the next few years. As this research unfolds, we'll have much clearer answers about who benefits most, which approaches work best, and how to maximize the durability of these remarkable treatment effects.
Frequently Asked Questions about Ketamine-Assisted Psychotherapy
How quickly can I expect results?
One of the most remarkable findings in ketamine assisted psychotherapy research is how quickly people start feeling better. Unlike traditional antidepressants that can take 6-8 weeks to kick in, ketamine works much faster.
Many people notice improvements within hours to days of their first session. In the healthcare provider study, participants reported better mood and daily functioning within just the first week.
However, the most significant and lasting changes typically unfold over multiple sessions spanning several weeks. Think of it like physical therapy—you might feel some relief after the first session, but the real change happens as you progress through the full program.
Is KAP safe for everyone?
While KAP shows tremendous promise, it's not a one-size-fits-all solution. The research has been careful about who should and shouldn't try this treatment.
KAP isn't recommended if you have:
- Active psychosis or severe mental health crises
- Serious heart problems or uncontrolled high blood pressure
- Certain other medical conditions that could make ketamine risky
This is why thorough medical and psychiatric evaluation is essential before starting treatment. When proper screening and monitoring are followed, serious problems are rare. You will likely experience some temporary effects during sessions—things like liftd blood pressure, some nausea, or feeling disconnected from your usual sense of reality. These effects are normal and typically fade within an hour or two.
Will I need maintenance sessions?
Most studies suggest an initial series of 3-6 sessions works best, typically spread over several weeks. This gives your brain time to form new patterns while the neuroplastic window is open.
After that initial series, maintenance needs vary from person to person. Many participants in long-term studies maintain their improvements for months after completing their initial series.
Some people find they benefit from occasional booster sessions—maybe every few months or when life stress increases. What seems to make the biggest difference is the integration therapy component. People who do the therapeutic work between sessions tend to go longer between needing additional ketamine sessions.
Conclusion
The transformative potential of ketamine assisted psychotherapy research is becoming impossible to ignore. Study after study shows that when we combine ketamine with skilled therapy, something remarkable happens—people who have struggled for years with treatment-resistant conditions finally find relief.
The numbers speak for themselves. 86% of PTSD patients no longer meeting diagnostic criteria. 65.8% alcohol abstinence rates at one year. These aren't just statistics—they represent real people who thought recovery might never be possible.
What excites me most about this research is how it challenges everything we thought we knew about healing timelines. Traditional therapy can take months or years to show progress. Psychiatric medications often require weeks to take effect, if they work at all. But ketamine opens what scientists call the "neuroplastic window"—a brief period when the brain becomes remarkably adaptable to change.
The evidence momentum is building across multiple conditions that have traditionally stumped mental health professionals. Depression that doesn't respond to antidepressants. PTSD that persists despite years of therapy. Addiction that keeps pulling people back despite their best efforts. The research shows that KAP offers hope where other treatments have fallen short.
At KAIR Program, we've watched this research evolve and incorporated these findings into our intensive retreat model. We've seen how combining ketamine with trauma-focused therapy in a supportive environment can create breakthrough moments that traditional weekly sessions might take months to achieve.
The research gaps that remain—larger studies, longer follow-up periods, more diverse populations—don't diminish what we already know. They simply point toward an even brighter future as scientists continue refining these approaches.
For people who have tried multiple treatments without success, ketamine assisted psychotherapy research offers something precious: evidence-based hope. The science is clear that when ketamine meets skilled psychotherapy in the right setting, remarkable healing becomes possible.
If you're curious about how these research findings translate into real-world treatment, our intensive retreat approach integrates cutting-edge science with compassionate, expert care designed for lasting change.
