Ketamine and Mood Disorders – A New Hope for Treatment-Resistant Conditions
Breaking Through: A New Frontier in Mood Disorder Treatment

Ketamine for mood disorders is rapidly emerging as a groundbreaking option for people who haven't responded to traditional treatments. If you're searching for quick information about this treatment approach, here's what you need to know:
| Ketamine for Mood Disorders: Key Facts |
|---|
| Effectiveness: ~70% response rate in treatment-resistant depression within hours to days |
| Speed: Works within 24 hours (vs. weeks for traditional antidepressants) |
| Conditions Treated: Major depression, treatment-resistant depression, bipolar depression, PTSD, anxiety, suicidality |
| Administration: IV infusion (most common), intranasal spray, subcutaneous injection, oral lozenges |
| Side Effects: Temporary dissociation, dizziness, mild blood pressure elevation |
| Duration: Effects typically last 1-2 weeks after a single treatment |
| Treatment Protocol: Usually 6 initial sessions over 2-3 weeks, then maintenance as needed |
Living with a treatment-resistant mood disorder can feel like being trapped in an endless cycle of suffering. Traditional antidepressants often take weeks to work—if they work at all—and for the approximately 30% of patients who don't respond to multiple medication trials, hope can seem distant.
That's where ketamine comes in. Originally developed as an anesthetic in the 1960s, this medication has shown remarkable ability to rapidly lift depression, reduce suicidal thoughts, and alleviate symptoms of various mood disorders—often within hours rather than weeks.
Unlike conventional antidepressants that target serotonin, norepinephrine, or dopamine, ketamine works on the glutamate system in the brain. This different mechanism appears to be why it can provide such quick relief, even in cases where other treatments have failed.
I'm Dr. Bambi Rattner, a psychologist specializing in trauma treatment who has witnessed the transformative potential of ketamine for mood disorders when integrated with appropriate psychotherapy. With over 30 years of clinical experience and specialized training in trauma healing, I've incorporated ketamine-assisted approaches into my intensive trauma retreats to help clients achieve breakthroughs that were previously unattainable.

How Ketamine Rewires the Brain
When we talk about ketamine for mood disorders, we're exploring a completely different approach to healing the mind. Unlike traditional antidepressants that slowly adjust serotonin or norepinephrine levels, ketamine works through the glutamate system—the brain's primary excitatory messenger.
The brain change that happens with ketamine is truly remarkable. Within minutes of receiving treatment, ketamine blocks special receptors called NMDA receptors on inhibitory neurons. This blockade creates a temporary "glutamate surge" throughout key brain regions. This surge activates AMPA receptors, triggering a cascade of healing signals that include the release of BDNF (Brain-Derived Neurotrophic Factor)—often called "fertilizer for the brain."
What happens next is what makes ketamine so revolutionary: your brain begins forming new connections, often within hours. These fresh neural pathways essentially "rewire" the circuits involved in mood regulation, creating what many researchers describe as a "reset" of brain networks that have become stuck in patterns of depression or anxiety.

The Science in Plain English
Imagine your brain as an intricate electrical system with billions of connections. In depression and anxiety, certain circuits become weakened or dormant—like neighborhoods experiencing a power outage. Traditional medications slowly restore power, street by street, which is why they take weeks to work.
Ketamine takes a more direct approach. It creates a brief but powerful surge of glutamate—like sending a reset signal throughout the system. This activates the brain's natural healing processes, particularly through something called the mTOR pathway (mammalian target of rapamycin).
When this pathway springs to life, it stimulates the proteins needed to build new connections between neurons. It's as if your brain can suddenly build bridges around the roadblocks created by depression. Many patients describe this sensation as a "fog lifting" or "seeing in color again" after their first treatment.
The dissociative effects that some people experience during treatment may also play an important role. This temporary shift in perception seems to help the brain break free from rigid thought patterns that maintain depression and anxiety.
Key Evidence Milestones
The story of ketamine for mood disorders is filled with breakthrough moments:
The journey began in 2000 when Dr. Robert Berman and his Yale colleagues published the first controlled study showing ketamine's rapid antidepressant effects. This was revolutionary—patients who hadn't responded to multiple medications were suddenly feeling better within hours.
By 2006, researchers at the National Institute of Mental Health confirmed these findings in treatment-resistant depression. The 2010s brought studies showing ketamine's effectiveness for suicidal thoughts, providing hope for crisis intervention. In 2016, large-scale research confirmed ketamine could help even in bipolar depression, which is notoriously difficult to treat.
A major milestone came in 2019 when the FDA approved esketamine (Spravato), a nasal spray derived from ketamine, for treatment-resistant depression. By 2020, esketamine received additional approval for depressive symptoms in adults with suicidal thoughts.
These findies represent a fundamental shift in mental health treatment. For the first time, we have a medication that can provide relief within hours rather than weeks—a true breakthrough for those who have struggled without relief. You can learn more about the scientific research on ketamine's neural connections through this informative video.
At KAIR Program, we've integrated these scientific insights into our approach, recognizing that ketamine's brain-rewiring effects are most powerful when combined with targeted therapeutic support.
Ketamine for Mood Disorders – What the Data Shows
The evidence supporting ketamine for mood disorders continues to grow, painting a picture of hope for many who've struggled with traditional treatments. As researchers dive deeper into this innovative approach, we're seeing impressive results across a spectrum of conditions.

How does "ketamine for mood disorders" work so fast?
Perhaps the most remarkable thing about ketamine is its speed. While conventional antidepressants often leave patients waiting 2-6 weeks for relief, ketamine frequently delivers significant improvement within just 24 hours of a single dose.
This isn't just anecdotal – science backs it up. In a pivotal controlled trial comparing ketamine to midazolam (which served as an active placebo), about 67% of people with treatment-resistant depression responded positively to ketamine within 24 hours. The midazolam group? Only 28% saw similar improvements.
For someone in the depths of depression, this rapid relief can be life-changing – or even life-saving. Studies show that about half of patients experiencing frequent suicidal thoughts before ketamine treatment reported a dramatic drop in those impulses afterward. Interestingly, this anti-suicidal effect often appears even before the full antidepressant benefits kick in, suggesting ketamine might have specific properties that directly target suicidal thinking.

Condition-by-Condition Snapshot
Major Depressive Disorder (MDD) responds remarkably well to ketamine, with 60-70% of patients showing improvement within 24 hours of a single infusion. Even more encouraging, 30-40% achieve complete remission after just one treatment. These effects typically last 3-7 days following a single session, which is why treatment protocols often include a series of infusions.
For those with Treatment-Resistant Depression (TRD) – folks who've tried multiple medications without success – ketamine offers renewed hope. After just three infusions over 11 days, studies show 52% of participants achieving complete remission, with another 15% showing partial response. Different infusion schedules show promise too, with response rates of 69% for twice-weekly sessions and 54% for three-times-per-week approaches.
Bipolar Depression has traditionally been challenging to treat, but ketamine is showing promise here as well. In one study of 42 patients with bipolar disorder, 52% responded positively to a single ketamine infusion. Another small study with 27 bipolar depression patients found that more than 48% responded within a week, and 37% reported full remission. What's particularly encouraging is that, when patients are properly screened, ketamine typically doesn't trigger manic episodes – a common concern with bipolar treatments.
Veterans and others suffering from PTSD have found remarkable relief through ketamine. One study of veterans with treatment-resistant depression and PTSD showed an astonishing 80% remission rate for PTSD symptoms after repeated ketamine infusions. The same research found a 93.3% response rate for depression symptoms. Many patients report that their trauma symptoms improve alongside their mood – a welcome dual benefit.
For those battling Anxiety Disorders, the research is still growing but looks promising. Early studies show response rates of 50-60% for conditions like generalized anxiety, social anxiety, and panic disorder. While the effects may not be quite as dramatic as those seen with depression, they're still significant enough to make a real difference in patients' lives.
Early research into Obsessive-Compulsive Disorder (OCD) shows potential for rapid symptom reduction, though these effects may be shorter-lived than with other conditions. While more studies are needed, case reports indicate real benefits for many OCD sufferers.
It's worth noting that many people with mood disorders also struggle with chronic pain. Since ketamine has well-established pain-relieving properties, patients often experience improvement in both their mental health and physical discomfort – a valuable dual benefit that few other treatments can offer.
Research from Yale Medicine continues to show promising results for ketamine as a breakthrough treatment, adding to the growing body of evidence supporting this innovative approach to mood disorders.
From Clinic to Couch: Treatment Journey
When you're considering ketamine for mood disorders, understanding what the full treatment journey looks like can help ease anxiety about the unknown. At KAIR Program, we believe treatment isn't just about medication—it's about creating a comprehensive healing experience custom to your unique needs.
Candidate Screening
Not everyone is an ideal candidate for ketamine therapy, which is why we take screening seriously. Think of this step as finding the right key for your specific lock.
A thorough screening typically starts with a psychiatric evaluation to confirm your diagnosis and review your treatment history. We'll also conduct a medical assessment to check for any contraindications like uncontrolled high blood pressure, review your medications for potential interactions, and perform a risk assessment for factors like psychosis risk or substance use concerns.
You might be a good fit for ketamine treatment if you've tried several conventional treatments without finding relief. Most of our clients have walked a long road of trial and error with traditional approaches before finding us.
Contrary to some misconceptions, having bipolar disorder doesn't automatically rule you out. When properly stabilized on mood-regulating medications, many bipolar patients safely benefit from ketamine with appropriate monitoring. Research shows that when screening is thorough, ketamine rarely triggers manic episodes.

Routes of Administration
Ketamine for mood disorders can be delivered in several ways, each with its own advantages—kind of like how you might prefer texting, calling, or face-to-face conversations for different situations.
Intravenous (IV) infusion is the most studied method, typically administered as 0.5 mg/kg over 40 minutes. It offers perfect bioavailability and precise dosing control, though it requires a medical setting and IV access. Think of this as the "gold standard" approach.
Intranasal delivery, FDA-approved as esketamine (Spravato), offers about 45% bioavailability. It's more convenient but requires monitoring in a clinical setting under the REMS program. The absorption can be a bit more variable than IV.
Subcutaneous injection is less common but quite effective with approximately 93% bioavailability. It's less invasive than IV but more than nasal spray, making it particularly helpful for older adults or those with difficult vein access.
Oral/sublingual lozenges have the lowest bioavailability (20-30%) but offer convenience, especially for maintenance therapy. Some providers prescribe these for at-home use, though higher doses may be needed to achieve similar effects.
At KAIR Program, we primarily use intramuscular (IM) ketamine during our intensive retreats. We've found this route provides reliable absorption while creating space for a more immersive therapeutic experience than IV administration allows.
Is "ketamine for mood disorders" right for me?
Fascinating research is emerging about who might respond best to ketamine. Surprisingly, people with a higher BMI often show better responses. Those with significant childhood trauma histories frequently experience more robust benefits, as do people with a family history of alcohol use disorder.
If you have anxious depression—depression with prominent anxiety features—you might be particularly responsive to ketamine therapy. On the flip side, certain genetic factors like BDNF gene variants may influence response, though this research is still developing.
Combining With Psychotherapy
At KAIR Program, we've seen how the magic really happens when ketamine for mood disorders is paired with skilled psychotherapy. This isn't just our opinion—research increasingly supports this combined approach.
Ketamine creates a window of increased brain plasticity—imagine your mind becoming temporarily more flexible and open to new perspectives. During this window, therapeutic interventions can take root more effectively. The mild dissociative state can also help you access difficult emotions or memories in a less threatening way, allowing for deeper processing.
Our trauma-focused intensive retreats leverage this unique synergy. We provide expert-led therapy sessions that make the most of ketamine's ability to temporarily loosen rigid thought patterns and defense mechanisms. The integration therapy we offer helps you make meaning from your ketamine experiences and extend the benefits far beyond what medication alone could achieve.
Many clients tell us that this combined approach helped them break through barriers they'd been struggling with for years in traditional therapy. It's not just about feeling better temporarily—it's about creating lasting change through a powerful combination of neurochemical shift and therapeutic insight.
For more information about our unique approach to ketamine-assisted healing, visit our ketamine retreats page.
Safety, Side Effects & Long-Term Considerations
When considering ketamine for mood disorders, it's natural to have questions about safety. At KAIR Program, we believe in transparent conversations about both the benefits and potential side effects of this powerful treatment option.
Short-Term Effects & Monitoring
During and shortly after a ketamine session, you might experience some temporary effects as your brain responds to the medication. Many people describe feeling "floaty" or disconnected from their surroundings – that's the dissociation effect that about 35% of patients experience.
You might also feel dizzy (quite common, happening for about 45% of people) or unusually drowsy (56% of patients report this). Some folks experience mild nausea (about 13%), and many notice changes in their blood pressure and heart rate during treatment. These physical changes are why we carefully monitor your vital signs before, during, and after each session.
Visual changes are also normal – you might notice colors appear more vibrant, patterns seem more interesting, or your vision might blur slightly. And that general feeling of things seeming "strange" or "unreal"? That's all part of how ketamine temporarily alters your perception.
The good news is that these effects typically fade within 1-2 hours after treatment. Our clinical team stays with you throughout this process, ensuring your comfort and safety every step of the way.

After your session, safety remains our priority. That's why we ask that you don't drive for at least 24 hours – your perception and reaction time might still be affected even when you feel normal. Having a trusted friend or family member with you after outpatient treatment provides both practical support and peace of mind.
It's also important to avoid alcohol and recreational drugs around your treatment time, as these can interact unpredictably with ketamine. Unless your doctor specifically directs otherwise, continue taking your prescribed psychiatric medications as usual.
Long-Term/Repetitive Use Risks
"What about the long-term effects?" This is one of the most common questions we hear, and it's an important one. Research on extended ketamine treatment is still evolving, but here's what we know so far:
When it comes to bladder and urinary tract health, the concerns you might have heard about mainly come from studies of recreational ketamine users who take extremely high doses frequently. At the controlled therapeutic doses we use for mood disorders, this risk appears minimal. That said, if you have pre-existing urinary issues, we'll monitor you more closely.
Cognitive effects are another area of interest. While some studies of long-term, high-dose recreational users show memory effects, patients receiving therapeutic doses typically don't experience significant cognitive impairment. In fact, many report thinking more clearly as their depression lifts – that mental fog that comes with depression often clears with successful treatment.
The question of tolerance and dependence deserves honest discussion. Physical dependence is possible but uncommon at therapeutic doses. The risk of psychological dependence is lower than with many other substances, though tolerance may develop over time, requiring adjustments to treatment schedules.
We also keep an eye on liver function, as rare cases of liver enzyme elevation have been reported. Routine monitoring helps us catch any concerns early.
When weighing these potential risks, it's crucial to consider them against the very real dangers of untreated severe depression – including profound suffering, deteriorating physical health, and sadly, suicide risk for many. For those who haven't found relief through traditional treatments, ketamine for mood disorders often represents hope when other options have failed.
At KAIR Program, our commitment to safety means individualized treatment plans, careful monitoring, and ongoing assessment of how the treatment is working for you – both the benefits and any side effects you might experience.
Practical Questions: Cost, Coverage, Choosing a Provider
Let's talk dollars and sense when it comes to ketamine for mood disorders. I know that practical concerns like cost and finding the right provider can feel overwhelming when you're already dealing with mental health challenges.
Cost and Coverage
The financial side of ketamine treatment varies quite a bit, and I want to be completely transparent about what you might expect:
For IV ketamine, most clinics charge between $400-$800 per infusion. Since the standard initial protocol typically involves 6 sessions over 2-3 weeks, you're looking at roughly $2,400-$4,800 for a complete initial treatment course.
If you're considering Spravato (the FDA-approved nasal esketamine spray), sessions generally run $590-$885 each. The silver lining here is that because Spravato has FDA approval, some insurance plans do provide partial coverage.
Maintenance treatments, which help sustain the benefits after your initial series, usually cost about the same as your initial sessions but happen less frequently—maybe once a month or as needed when symptoms return.
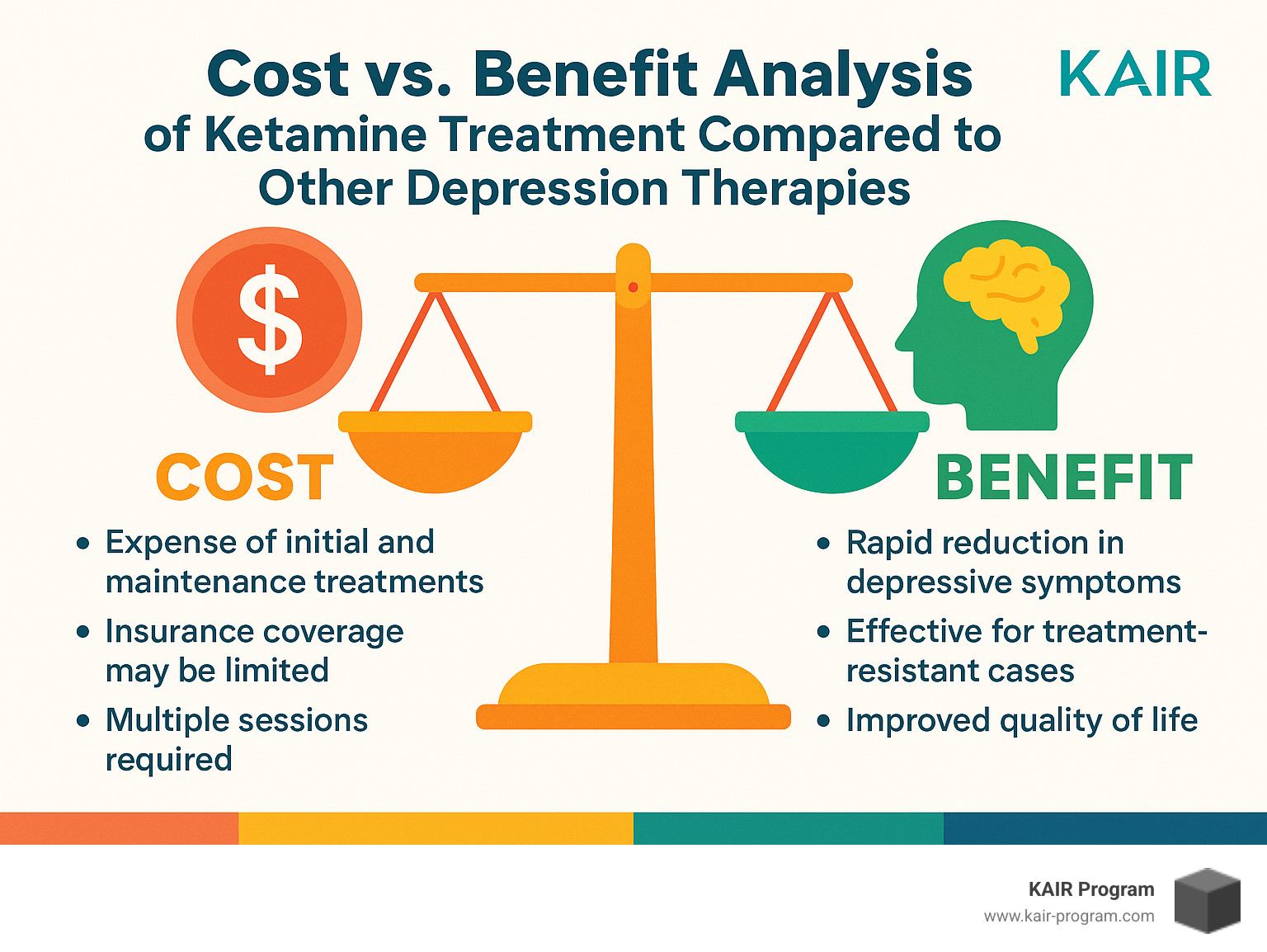
The insurance landscape is slowly changing, but there's still a way to go. Most insurance plans don't cover IV ketamine for psychiatric conditions yet, though Spravato has better coverage odds. To qualify for coverage, you'll typically need to document "treatment resistance"—essentially proving you've tried multiple conventional treatments without success.
At KAIR Program, our ketamine-assisted intensive retreats have a different pricing structure because we're combining ketamine for mood disorders with comprehensive trauma therapy in an immersive format. While the upfront cost may be higher than individual infusions, many clients find the value proposition compelling when considering the depth of treatment provided.
Choosing a Provider
Finding the right ketamine provider is a bit like dating—chemistry matters, and you want someone who really gets you. Here's what to look for:
Medical Expertise: Ideally, your treatment should involve a psychiatrist or mental health professional who can properly evaluate your condition and monitor your progress. Ask if the staff is trained in Advanced Cardiovascular Life Support (ACLS) and what kind of screening they perform before treatment. Good providers conduct thorough medical and psychiatric evaluations, not just quick consultations.
Treatment Approach: Some clinics offer ketamine as a standalone treatment, while others (like us at KAIR) integrate it with therapy. Research suggests that combining ketamine for mood disorders with appropriate therapeutic support may lead to more lasting benefits. Ask about personalized treatment plans and protocols for both initial treatment and maintenance.
Facility and Comfort: The environment matters more than you might think. When you're in a ketamine session, you're vulnerable and open. The treatment space should feel safe, comfortable, and private. Good providers have proper monitoring equipment and clear emergency protocols.
Integration Support: This is often overlooked but critically important. The ketamine experience can bring up profound insights and emotions. Does the provider offer guidance for processing these experiences? Are follow-up appointments included? Is there support available between treatments?
At KAIR Program, we've seen that the combination of ketamine for mood disorders with expert-led trauma therapy creates a powerful synergy. The ketamine helps "unstick" rigid neural patterns, while the therapy helps you build new, healthier patterns in their place.
Comparing Alternatives
You might be wondering how ketamine stacks up against other treatment options:
Compared to traditional antidepressants, ketamine for mood disorders works much faster (hours instead of weeks) and has a higher response rate for treatment-resistant cases. The side effects are different—less sexual dysfunction and weight gain, but more dissociation and dizziness during treatment. Ketamine does require more frequent administration initially.
Versus ECT (electroconvulsive therapy), ketamine is significantly less invasive with fewer cognitive side effects. While ECT might have a slight edge for severe depression, ketamine doesn't carry the same anesthesia risks or memory concerns.
When compared to TMS (transcranial magnetic stimulation), ketamine offers faster onset and requires fewer initial sessions. The immediate effects are more noticeable, though long-term efficacy seems similar.
As for psychotherapy alone, ketamine provides more rapid symptom relief and addresses biological aspects directly. That said, we've found the best results often come from combining both—using ketamine to create a window of neuroplasticity and therapy to help reshape thought patterns during that window.
There's no one-size-fits-all approach to mental health. The right treatment for you depends on your specific symptoms, history, preferences, and goals. We're always happy to discuss whether our ketamine-assisted intensive retreats might be a good fit for your healing journey.
Frequently Asked Questions about Ketamine Treatment
What happens during a ketamine session?
Wondering what to expect during treatment? At KAIR Program, we've designed our ketamine for mood disorders sessions to be both therapeutic and comfortable.
Your session begins with a gentle preparation phase where we check your vital signs and conduct a brief psychological check-in. This is a great time to set intentions for your experience. We believe this mindful preparation helps create the foundation for meaningful healing.
When you're ready, we administer the ketamine—typically through the intramuscular route at our retreats. Unlike the drawn-out waiting period with traditional antidepressants, ketamine begins working within minutes, with effects reaching their peak around the 15-25 minute mark.
Throughout your journey, our compassionate clinicians remain by your side. We're not just monitoring your physical response—we're providing a supportive presence as you steer the experience. As the effects gradually subside over 1-2 hours, we begin the initial processing together.
"The ketamine experience feels different for everyone," explains Dr. Rattner. "Some people describe feeling peacefully detached from their body, while others notice visual changes or find themselves connecting with emotions in new ways. Even the occasionally uncomfortable dissociative effects seem to play an important role in the healing process."
The experience doesn't end when the medication wears off. Our structured integration therapy helps you make meaning of your experience, changing insights into lasting change.
How long will benefits last and will I need boosters?
One of the most common questions we hear is about the staying power of ketamine for mood disorders treatment. The honest answer? It varies from person to person.
After a single treatment, most people maintain benefits for about 3-7 days. Following our recommended series of six infusions, many patients enjoy improvements that last 2-4 weeks or longer. Some find they need maintenance sessions every 2-6 weeks to sustain their progress, while others experience lasting relief for months without additional treatment.
Several factors influence how long your benefits might last:
- The severity and duration of your mood condition
- What other medications or therapies you're using
- Lifestyle elements like sleep quality, stress levels, and substance use
- Your unique biological makeup
What sets KAIR Program apart is our integration of intensive therapy with ketamine treatment. We've consistently found that this combined approach produces more durable results than medication alone. Many of our clients need fewer maintenance sessions over time, and some find they no longer need them at all.
Can ketamine trigger mania in bipolar disorder?
If you're living with bipolar disorder, you might worry about treatment triggering a manic episode. It's a valid concern, but the research is reassuring when proper precautions are taken.
Most studies show that ketamine for mood disorders carries a low risk of triggering mania in stabilized bipolar patients. The key word here is "stabilized"—we recommend maintaining your prescribed mood stabilizers during ketamine treatment rather than discontinuing them.
Morning administration can help reduce sleep disruption (a potential mania trigger), and our team closely monitors for any early signs of mood elevation throughout your treatment journey.
For our bipolar clients, we typically recommend:
- Continuing stable doses of mood stabilizers before starting ketamine
- Scheduling treatment during depressive episodes, not during or immediately after manic periods
- Administering treatment in the morning when possible
- Regular mood monitoring before, during, and after each session
With these precautions in place, many of our bipolar clients have found ketamine to be a valuable tool for managing depressive episodes without triggering the mood pendulum to swing too far in the opposite direction.
Conclusion
Ketamine for mood disorders stands as one of the most remarkable breakthroughs we've seen in psychiatric treatment in decades. If you've been struggling with treatment-resistant depression, bipolar depression, PTSD, or other stubborn mood disorders, ketamine offers something truly precious that might have felt out of reach: rapid relief and a renewed sense of hope.
The science speaks volumes. With response rates of 60-70% in treatment-resistant cases, quick reduction in suicidal thoughts, and benefits spanning multiple mood disorders, ketamine's potential is nothing short of remarkable. While it's not a magic bullet for everyone, ketamine provides a powerful tool that can break through the suffocating cycle of severe depression and create a genuine window of opportunity for deeper healing.
Here at KAIR Program, we've had the privilege of witnessing truly transformative changes in our clients who combine ketamine with intensive trauma-focused therapy. There's something special that happens when ketamine's ability to improve neuroplasticity and temporarily loosen those rigid thought patterns meets expert-guided therapy. Our retreats create a safe environment where deep healing can unfold in a surprisingly compressed timeframe – often achieving breakthroughs that might otherwise take years of conventional therapy.
The landscape of ketamine for mood disorders continues to evolve in exciting ways. Researchers are actively exploring biomarkers that might predict who will respond best, fine-tuning optimal dosing protocols, and developing ketamine analogs that might offer the same benefits with fewer side effects. Meanwhile, thousands of real people are already experiencing life-changing relief through this innovative approach.
If you've been struggling with a mood disorder that hasn't responded well to traditional treatments, ketamine may offer a meaningful path forward. We encourage you to have an open conversation with your healthcare providers about whether this option might be right for you. And consider whether a comprehensive approach like our ketamine-assisted intensive retreats at KAIR Program might be the integrative solution you've been searching for.
Even in what feels like the darkest moments of depression or trauma, breakthrough treatments like ketamine remind us that healing is possible—sometimes arriving more rapidly than we ever dared to hope. Your brain has an incredible capacity for healing and renewal, and ketamine for mood disorders might just be the catalyst that helps open up that potential.
More info about ketamine retreats
