Healing PTSD with Ketamine – What You Need to Know
Breaking the Cycle of Trauma: A New Approach

Ketamine for PTSD treatment represents a groundbreaking approach for those who have struggled with post-traumatic stress disorder and found limited relief through conventional therapies. This innovative treatment offers hope for many who feel stuck in their healing journey.
Quick Facts About Ketamine for PTSD:
- Acts rapidly, often providing relief within hours (unlike traditional medications that take weeks)
- Works by promoting new neural connections in the brain
- Administered via IV infusion, intranasal spray, or as part of psychotherapy
- Success rates of 50-70% in treatment-resistant PTSD cases
- Typically requires a series of 6 initial treatments followed by maintenance sessions
For many trauma survivors, traditional treatments like SSRIs (selective serotonin reuptake inhibitors) and exposure therapy don't provide adequate relief. Ketamine for PTSD treatment works differently by targeting the glutamate system rather than serotonin, potentially "resetting" traumatic memory patterns and reducing hypervigilance.
The journey toward healing from PTSD can feel overwhelming, especially when previous treatments haven't delivered the relief you deserve. Ketamine offers a different pathway - one that addresses the neurobiological underpinnings of trauma while creating space for psychological healing.
I'm Dr. Bambi Rattner, a psychologist with experience in trauma treatment who has witnessed how ketamine for PTSD treatment can create breakthrough moments for clients when traditional approaches have fallen short. My practice integrates ketamine treatment with trauma-focused therapy to provide comprehensive healing for those seeking relief from PTSD symptoms.

Understanding Post-Traumatic Stress Disorder
When we talk about PTSD, we're discussing much more than just bad memories that linger. This condition rewires the brain's very architecture, fundamentally changing how a person processes everyday information, manages emotions, and responds to stress. Before we explore how ketamine for PTSD treatment can help, it's important to understand what's actually happening in the brain and body of someone experiencing post-traumatic stress.
What Is PTSD and Who Is Affected?
The DSM-5 (the diagnostic bible of mental health) defines PTSD as a condition that develops after exposure to actual or threatened death, serious injury, or sexual violence. This trauma can be experienced directly, witnessed firsthand, learned about happening to someone close, or from repeated exposure to traumatic details – something first responders know all too well.
PTSD manifests through four main symptom clusters that can truly hijack a person's life:
- Vivid re-experiencing of the trauma through flashbacks and nightmares
- Deliberate avoidance of anything that might trigger trauma memories
- Negative changes in thoughts and mood, often including shame or detachment
- Heightened arousal, leaving people constantly on edge, easily startled, and exhausted
About 7-8% of Americans will experience PTSD during their lifetime. While combat veterans often come to mind first (with 11-20% of Iraq and Afghanistan veterans developing the condition), PTSD touches lives across all backgrounds and experiences. Sexual assault survivors face particularly high risks, with approximately half developing PTSD. The condition also affects childhood abuse survivors, accident victims, witnesses to violence, and those who've experienced medical trauma.

At its core, PTSD involves a dysregulated stress response system. The brain and body get stuck in survival mode, with abnormal cortisol patterns and disrupted glutamate signaling creating a biological cycle that's difficult to break. Clinicians often use tools like the PCL-5 (PTSD Checklist) to measure symptom severity and track how well treatments are working.
Limitations of Current Standard Treatments
Traditional PTSD treatments have certainly helped many people reclaim their lives, but they come with significant limitations that can leave many still suffering:
SSRIs like sertraline and paroxetine are FDA-approved for PTSD, but the reality is they only achieve full remission in about 20-30% of patients. They typically require 4-6 weeks before showing any benefit, and many people struggle with side effects like sexual dysfunction, weight changes, and emotional numbness – sometimes feeling like trading one problem for another.
Prazosin can help reduce the nightmares that often torment people with PTSD, but results vary widely from person to person, and it doesn't address the full spectrum of symptoms that make daily life so challenging.
Trauma-focused psychotherapies like Prolonged Exposure and Cognitive Processing Therapy have strong evidence behind them, but they require directly confronting traumatic memories – something so distressing that 30-40% of patients drop out before completing treatment. For many, the short-term distress feels too overwhelming, even with the promise of long-term relief.
EMDR therapy has helped many process traumatic memories, but it doesn't work for everyone and typically requires multiple sessions over weeks or months before benefits appear – a long wait when someone is suffering intensely.
These limitations create a significant treatment gap, especially for those with severe or treatment-resistant PTSD. This is precisely where ketamine for PTSD treatment offers new hope as a promising alternative with a completely different mechanism of action and potential for rapid relief.
How Ketamine Works in the Brain
The science behind ketamine for PTSD treatment offers a approach to healing trauma at its neurobiological roots.

When ketamine enters your brain, it triggers a fascinating cascade of healing processes. Unlike traditional medications that focus on serotonin, ketamine works primarily as an NMDA receptor blocker. Think of these receptors as doors that glutamate (an excitatory brain chemical) normally passes through. When ketamine temporarily blocks these doors, something remarkable happens – a surge of glutamate is released elsewhere in the brain.
This glutamate surge isn't random chaos – it's the beginning of a healing journey. It activates AMPA receptors, which then kickstart the brain's natural repair system through something called the mTOR pathway. This pathway is like turning on your brain's construction crew, leading to increased production of Brain-Derived Neurotrophic Factor (BDNF) – essentially brain fertilizer that helps grow new connections.
Within hours – not weeks or months like traditional medications – ketamine for PTSD treatment stimulates the formation of new synaptic connections, particularly in brain regions damaged by trauma and chronic stress. Your prefrontal cortex and hippocampus, areas critical for emotional regulation and memory processing, begin to rebuild and reconnect.
As an added benefit, ketamine reduces neuroinflammation, which is often liftd in people with PTSD and contributes to many troubling symptoms. This comprehensive approach addresses the glutamate dysregulation that plays a central role in how trauma impacts the brain.
For a deeper scientific understanding of these processes, you might want to explore this research on ketamine neurobiology.
Reconsolidation and Fear Memory Disruption
One of the most promising aspects of ketamine for PTSD treatment is how it affects traumatic memories themselves.
When you recall a traumatic memory, it temporarily enters a vulnerable state before being stored again – a process called reconsolidation. Ketamine appears to interrupt this process by inhibiting necessary protein synthesis in the amygdala (your brain's fear center). This creates a unique opportunity where painful memories can potentially be "updated" with new, less threatening information.
Think of it as opening a document, making edits, and saving the changes – rather than the original file remaining permanently unchanged. This mechanism helps explain why combining ketamine with trauma-focused therapy can be so powerful. The medication creates a brain state where therapeutic insights can have deeper, more lasting impacts on memory structures.
Ketamine also improves extinction learning – your brain's ability to learn that something once perceived as dangerous no longer poses a threat. This combination of effects helps break the cycle of trauma that keeps many PTSD sufferers trapped in their past.
Speed of Symptom Relief
Perhaps the most remarkable feature of ketamine for PTSD treatment is how quickly it works. While traditional medications often leave patients waiting weeks for relief:
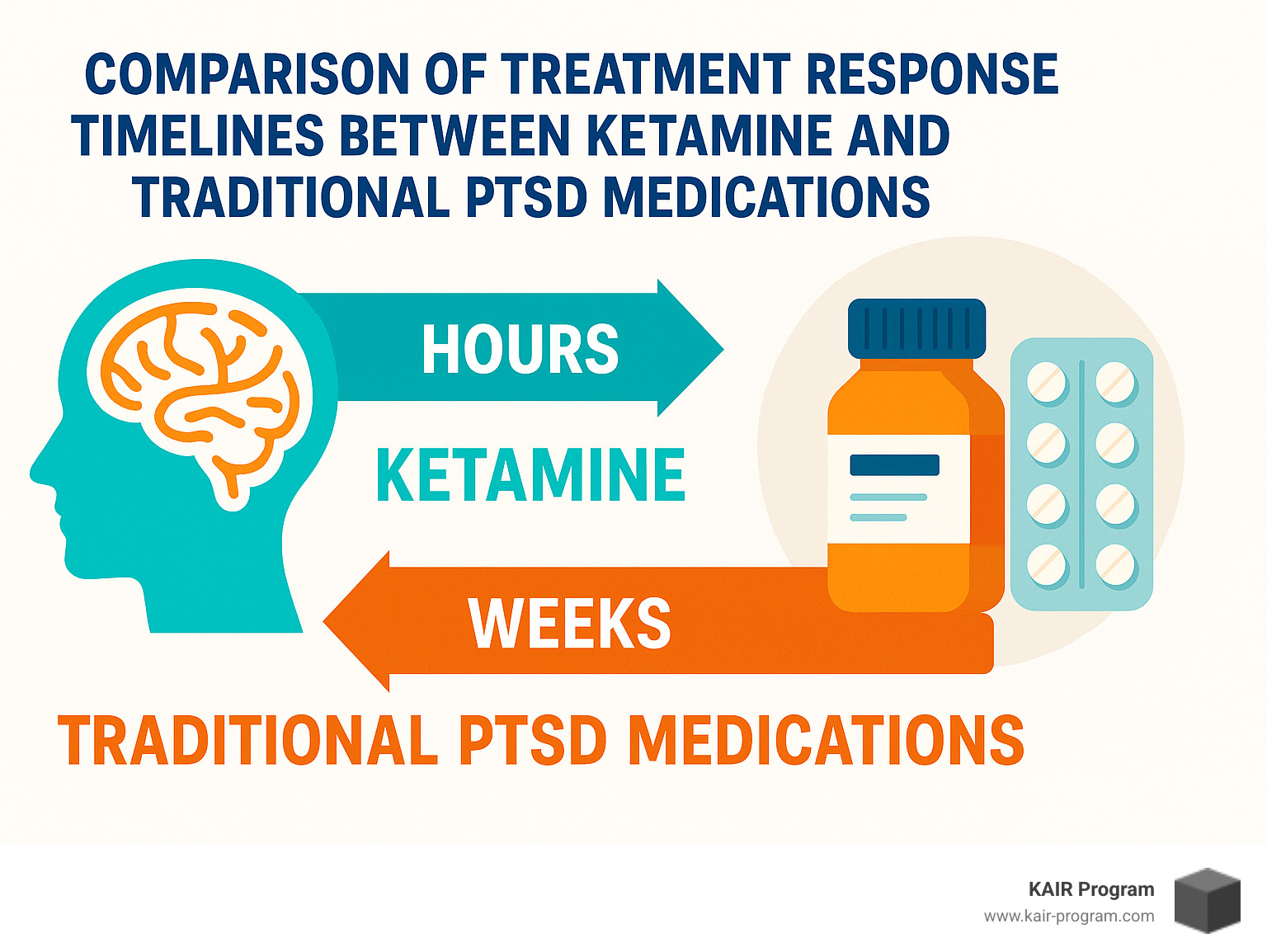
Many people experience significant symptom reduction within hours of their first ketamine session. Research shows measurable drops in PCL-5 scores (the standard tool for measuring PTSD symptoms) within just 24 hours of treatment. For someone who's been suffering for years, sometimes decades, this rapid relief can feel nothing short of miraculous.
This quick action is particularly valuable for people in acute distress or with suicidal thoughts. When you've been fighting an exhausting battle with treatment-resistant PTSD, having a treatment that doesn't make you wait weeks to feel better can be life-changing – and sometimes life-saving.
The brain science behind ketamine for PTSD treatment represents a fundamental shift in how we understand and treat trauma – addressing both the neurochemical imbalances and the painful memories that keep people stuck in cycles of suffering.
Ketamine for PTSD Treatment
Now that we understand how ketamine works in the brain, let's explore the practical aspects of ketamine for PTSD treatment – including administration methods, protocols, and what patients can expect.
When it comes to receiving ketamine treatment, you have several options. The most common approach is through intravenous (IV) infusion, where ketamine is administered at approximately 0.5 mg/kg over a 40-minute session. This method gives medical providers precise control over dosing and allows for immediate oversight of your experience.
Some patients might receive intranasal esketamine (Spravato) instead. While FDA-approved specifically for treatment-resistant depression, many clinicians use it off-label for PTSD with promising results. There are also less common but still effective routes like oral ketamine (sometimes used between infusions as maintenance) and intramuscular (IM) injections which work faster than oral administration but offer less control than IV methods.
Most people who try ketamine for PTSD treatment follow a similar journey: an initial series of six infusions spread across 2-3 weeks, followed by an assessment to measure improvement, and then maintenance treatments every 2-4 weeks as needed. The good news? Studies show that 50-70% of patients experience significant symptom reduction – even those who've tried multiple conventional treatments without success.
Ketamine Infusion Therapy: What to Expect
Walking into your first ketamine session can feel intimidating, but understanding the process helps ease those pre-treatment butterflies.
Your visit will begin with a brief check-in where providers measure your vital signs and have you complete symptom questionnaires. They'll review your medical history to ensure ketamine remains appropriate for you. Then you'll settle into a comfortable reclining chair in a quiet, calming space – many clinics offer eye masks and gentle music to improve relaxation.
A small IV line is placed in your arm, and monitoring equipment tracks your heart rate, blood pressure, and oxygen levels throughout your 40-minute treatment. As the ketamine enters your system, you'll likely experience a gentle sense of dissociation or detachment from your body. Some people notice visual changes, altered time perception, or emotional insights emerging. The most intense effects typically last just 10-15 minutes, and many patients describe this experience not as frightening but as interesting, insightful, or even peaceful.
After your infusion ends, you'll remain at the clinic for 30-60 minutes as the immediate effects subside. Most people feel clear-headed enough to head home within an hour – though you'll need someone else to drive you.
Ketamine-Assisted Psychotherapy vs Infusion Alone
While ketamine infusions by themselves can significantly reduce PTSD symptoms, pairing ketamine with specialized therapy often creates deeper, longer-lasting healing. This combination approach, known as Ketamine-Assisted Psychotherapy (KAP), works through several frameworks.
The TIMBER Model (Trauma Interventions using Mindfulness Based Extinction and Reconsolidation) weaves together ketamine treatment with mindfulness practices and trauma processing. Other approaches combine Prolonged Exposure therapy with ketamine, leveraging the medication's ability to reduce fear responses while improving learning and neuroplasticity.
Many practitioners, including our team at KAIR Program, focus on integration-focused approaches where the insights generated during ketamine sessions are carefully processed with a therapist afterward. These integration sessions help you make meaning from your experience and apply these realizations to your everyday life.
At KAIR Program, we've developed ketamine-assisted intensive retreats that combine the biological benefits of ketamine with expert-led trauma therapy. This comprehensive approach addresses both the brain chemistry aspects and the psychological dimensions of PTSD, creating opportunities for profound healing.
Who Is an Ideal Candidate for Ketamine for PTSD Treatment
Ketamine for PTSD treatment isn't for everyone, but it can be transformative for the right patients. You might be an excellent candidate if you have treatment-resistant PTSD and haven't found adequate relief from at least two conventional treatments. People experiencing both PTSD and depression often respond particularly well, as ketamine effectively addresses both conditions simultaneously.
If you're struggling with suicidal thoughts, ketamine's rapid anti-suicidal properties make it an especially valuable option. Those who experience significant side effects from traditional PTSD medications may also find ketamine more tolerable.
However, safety comes first. Ketamine isn't appropriate for everyone, particularly those with uncontrolled hypertension, unstable cardiovascular disease, history of psychosis, pregnancy, active substance abuse, or severe liver disease. That's why a thorough medical screening is essential before beginning treatment.
The journey of healing from trauma is deeply personal, and finding the right treatment approach matters. For many who've struggled for years with persistent PTSD symptoms, ketamine for PTSD treatment offers a new pathway toward relief – one that works differently than conventional approaches and may succeed where others have fallen short. More info about ketamine-assisted retreats
Safety, Risks, and Practical Considerations
When you're considering ketamine for PTSD treatment, it's natural to have questions about safety, side effects, and the practical matters that affect your decision. Let's walk through what you need to know to make an informed choice.
Safety Profile and Common Side Effects
Ketamine has been a trusted medical tool for over five decades, primarily as an anesthetic. The good news is that the doses used for PTSD treatment are much lower than those used in surgery, which contributes to its safety when used properly.
During and shortly after your ketamine session, you might experience some temporary effects. Your blood pressure and heart rate may increase for a short time. About one in five people feel some nausea. You might feel dizzy or "spacey," experience a sense of detachment from your body (that's the dissociative effect), have slightly blurred vision, or develop a headache.
Don't worry—these effects typically fade within an hour or two after treatment. When administered by qualified medical professionals with proper monitoring, serious adverse events are quite rare.
For the longer term, there are a few considerations to keep in mind. With frequent, long-term ketamine use, some people experience bladder irritation, though this is rarely seen with the frequency and dosage used for PTSD treatment. Your provider might recommend periodic liver function monitoring. And a small percentage of patients may develop psychological dependence, which is why treatment is carefully structured and monitored.
Cost and Insurance Considerations
The financial aspect of ketamine for PTSD treatment remains one of its biggest challenges:
IV ketamine infusions typically range from $400-$800 per session, with a complete initial series of six infusions potentially costing between $2,400-$4,800. Then there are maintenance infusions every 2-4 weeks to consider for ongoing care.
Unfortunately, most insurance plans don't cover ketamine infusions for PTSD since this remains an off-label use. Some plans do cover intranasal esketamine (Spravato) for treatment-resistant depression, which may help if you're dealing with both PTSD and depression.
At KAIR Program, we understand these financial realities and strive to make our ketamine-assisted retreats as accessible as possible. We're always transparent about pricing and can help you explore potential payment options that might work for your situation.
Legal Status and Accessibility
In the United States, ketamine is classified as a Schedule III controlled substance—legally available for medical use with a prescription, but with restrictions to prevent misuse.
Only licensed physicians can prescribe ketamine, and IV infusions must take place in a medical setting. While prescribing ketamine "off-label" for PTSD is both legal and increasingly common, availability varies significantly depending on where you live. Urban areas typically offer better access to ketamine providers than rural regions.
Managing Side Effects and Maximizing Benefits
To get the most from your ketamine for PTSD treatment while keeping discomfort to a minimum, consider these helpful approaches:
Before your treatment, try fasting for 4-6 hours to reduce the chance of nausea. Practice simple mindfulness techniques that can help guide your experience during treatment. Many people find it helpful to set intentions for their session—what healing or insights you hope to gain. And don't forget to arrange transportation, as you cannot drive for 24 hours after treatment.
During your session, keep open communication with your provider about your comfort level. If nausea becomes an issue, anti-nausea medication can usually be provided. Rather than fighting the dissociative experience, most people find it more beneficial to surrender to it.
After treatment, consider journaling about your insights and experiences while they're fresh. Participating in integration therapy sessions can help you process and apply what you've learned. Continue with supportive treatments like talk therapy, and maintain healthy lifestyle habits to extend the benefits of your ketamine treatment.
Research Gaps & Future Directions for Ketamine for PTSD Treatment
While the current research on ketamine for PTSD treatment shows great promise, important questions remain unanswered.
Most studies only follow patients for weeks or months, leaving us with limited data on long-term outcomes. Questions about ideal dosing, frequency, and treatment duration are still being explored. Researchers are investigating potential biomarkers (like d-serine levels) that might help predict who will respond best to ketamine. And we need larger studies on the most effective ways to combine ketamine with various psychotherapy approaches.
The good news is that the field is evolving rapidly. Several large randomized controlled trials are currently underway that will help answer these questions and potentially expand access to this promising treatment.
At KAIR Program, we stay closely connected to emerging research to ensure our retreat programs incorporate the latest findings about ketamine for PTSD treatment, offering you the most effective healing experience possible. Our approach combines the biological benefits of ketamine with expert-led trauma therapy to address both the neurobiological and psychological aspects of PTSD.
Frequently Asked Questions about Ketamine for PTSD
How long do benefits from ketamine for PTSD treatment last?
One of the most common questions we hear relates to how long the relief will last. The truth is, everyone's journey with ketamine for PTSD treatment is unique.
After completing an initial series of infusions, some people find their improvements last for several weeks or even months without additional treatment. For most, however, the benefits gradually begin to fade, signaling the need for maintenance sessions every 2-4 weeks.
We've noticed at KAIR Program that patients who combine their ketamine treatments with meaningful psychotherapy often experience longer-lasting benefits. The medication opens a window of neuroplasticity, and therapy helps cement those positive changes.
Your personal duration of relief may depend on several factors: the severity of your trauma history, whether you're facing ongoing stressors in your life, and simply your individual brain chemistry. That's why we create personalized maintenance plans for each person based on their unique response pattern rather than following a one-size-fits-all approach.
Can I drive after an infusion?
The short answer is absolutely not. Even after the dreamlike, dissociative effects of ketamine have faded, the medication continues to affect your coordination, reaction time, and perception for at least 24 hours.
I remember one patient who felt "completely normal" an hour after treatment but then tried to pour coffee and completely missed the cup! Your brain needs time to fully process the experience, and during that time, driving would be dangerous for both you and others on the road.
Always arrange for someone to drive you home after your ketamine for PTSD treatment session. This could be a friend, family member, or a rideshare service—whatever works best for you. At KAIR Program, we won't begin treatment until we've confirmed you have safe transportation home.
Will ketamine replace my current medications?
Ketamine for PTSD treatment typically works alongside your existing medication regimen, at least initially. We don't recommend stopping any psychiatric medications without carefully consulting the doctor who prescribed them.
Many of our patients continue taking their regular antidepressants, mood stabilizers, or anxiety medications throughout their ketamine treatment journey. Some find that after successful ketamine therapy, they're able to gradually reduce or even discontinue certain medications—but this should always be done slowly and with proper medical oversight.
It's worth noting that certain medications, particularly benzodiazepines (like Xanax or Klonopin) and lamotrigine (Lamictal), may reduce ketamine's effectiveness. Your provider might recommend adjusting the timing or dosage of these medications before your treatment.
At KAIR Program, we believe in collaborative care. Your ketamine provider should work closely with your primary psychiatric provider to create a coordinated treatment plan that addresses all aspects of your mental health.
Is ketamine treatment addictive?
This is an understandable concern given ketamine's history. When used at therapeutic doses and frequencies specifically for PTSD treatment, addiction is rare. The controlled medical application of ketamine for PTSD treatment is fundamentally different from recreational use in both dosage and context.
Before beginning treatment, we carefully screen all patients for substance use disorders. All treatments take place in controlled medical settings with proper monitoring. Unlike some medications, patients don't receive ketamine to take home (with rare exceptions for carefully monitored oral ketamine in some practices).
Our treatment protocols include regular check-ins to watch for any problematic use patterns. We take this aspect of care seriously because our goal is healing, not creating new challenges for our patients.
How quickly will I know if ketamine is working for my PTSD?
Many patients experience noticeable effects after their very first infusion, which can be incredibly encouraging after years of struggling with traditional treatments that take weeks to show benefits.
The timeline typically looks something like this: reduction in intrusive thoughts and nightmares often comes first, sometimes within hours of treatment. Improvements in mood and anxiety frequently follow close behind. The hypervigilance and exaggerated startle response that make everyday life so challenging with PTSD may take a bit longer to improve.
By the third or fourth infusion, most people who are going to respond to ketamine for PTSD treatment will show significant symptom reduction. We use standardized assessment tools throughout your treatment to objectively track your progress, rather than relying solely on subjective feelings.
One patient described it beautifully: "It wasn't that my memories changed—they're still there. But they don't ambush me anymore. I can think about what happened without being dragged back into it. For the first time in years, I feel like I'm living in the present."
Conclusion
When trauma feels like it's woven into the fabric of your daily life, finding a path forward can seem impossible. That's why ketamine for PTSD treatment represents such a meaningful breakthrough for many who've struggled to heal through conventional approaches alone.
At KAIR Program, we've been privileged to witness profound changes in people who arrived feeling that their trauma was impossible. Our ketamine-assisted intensive retreats create a unique healing environment where the neurobiological reset that ketamine provides works hand-in-hand with expert trauma therapy. This dual approach addresses both the brain chemistry that keeps trauma locked in place and the psychological healing needed to move forward.
What makes ketamine for PTSD treatment so remarkable is its potential to create relief within hours – not the weeks or months required by traditional medications. For someone who has lived with hypervigilance, nightmares, and emotional numbness for years, this rapid shift can feel like finally taking a full breath after being underwater.
This window of neuroplasticity does something precious – it creates space for new possibilities. When the brain becomes more receptive to change, trauma-focused therapy can help rewrite narratives that once seemed permanently etched in stone.
Of course, ketamine for PTSD treatment isn't a one-size-fits-all solution. It doesn't work for everyone, and it's not a standalone cure. But for many who've felt stuck in their healing journey, it offers a different doorway – one that bypasses the roadblocks that have made traditional treatments ineffective.
The journey through trauma is never simple, but it doesn't have to be endless. With approaches like ketamine-assisted therapy, many people find that healing becomes not just possible but tangible. At KAIR Program, we're committed to walking alongside you on this journey, bringing together the best of innovative medicine and compassionate therapy to light the way forward.
If you or someone you care about has been struggling with treatment-resistant PTSD, we invite you to learn more about our ketamine-assisted retreats. Our team understands the courage it takes to try something new after disappointments, and we're here to answer your questions and help you find if this approach might be your next step toward healing.

