Ketamine Therapy Explained: Healing Trauma One Infusion at a Time
A New Hope: Ketamine for Trauma Therapy

If you're seeking profound relief from the lingering effects of trauma, you're not alone. Ketamine for trauma therapy is an emerging and powerful approach offering new hope.
What is Ketamine for Trauma Therapy?
- Approach: Uses low doses of ketamine, often combined with psychotherapy.
- Goal: Helps individuals with Post-Traumatic Stress Disorder (PTSD) and other trauma-related conditions.
- Benefit: Aims for rapid relief and deeper healing, especially for those who haven't responded to traditional treatments.
- How it works (briefly): Believed to promote new neural connections and help process traumatic memories with less fear.
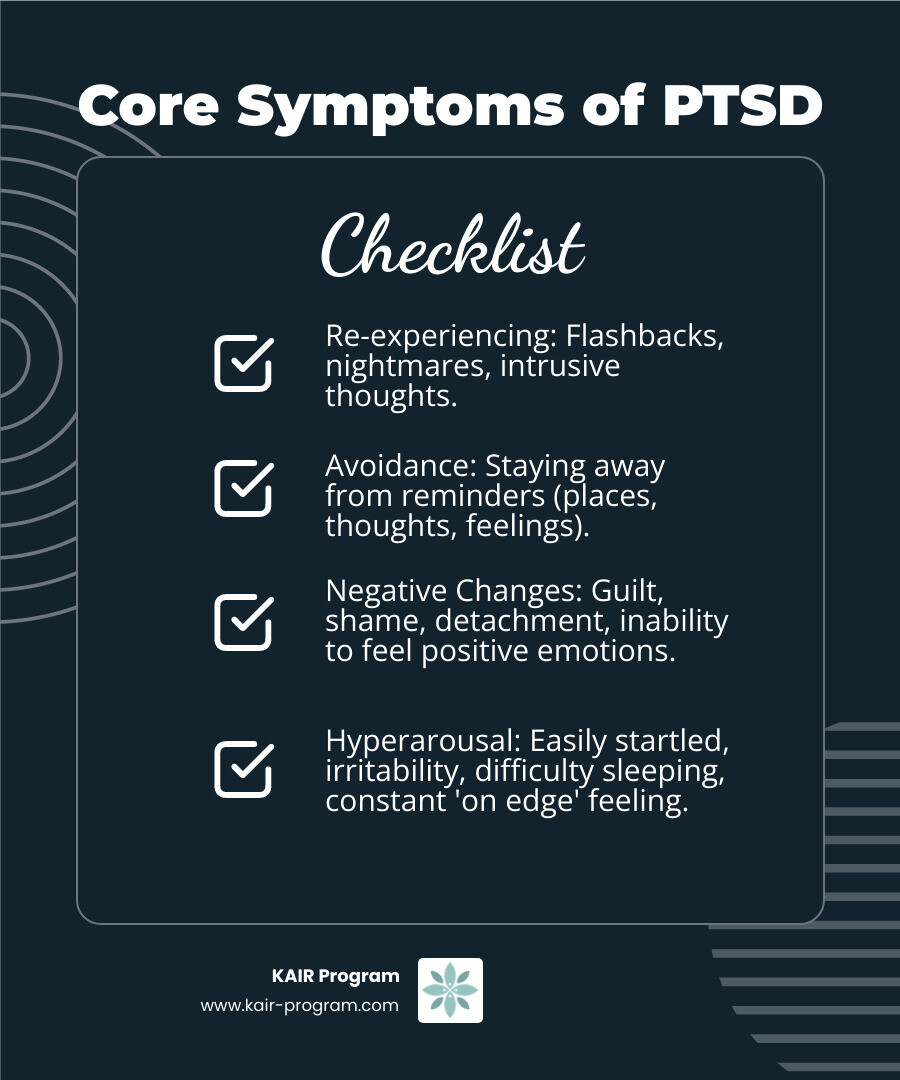
Life after trauma can feel like an endless struggle. Millions of people worldwide grapple with the invisible wounds of Post-Traumatic Stress Disorder (PTSD). Studies show that the lifetime prevalence of PTSD in the general population can be as high as 9%. This condition can make daily life incredibly challenging, marked by constant hypervigilance, emotional numbness, and difficulty connecting with others.
Traditional therapies and medications offer help for many. But for a significant number, symptoms persist. The average dropout rate for trauma-specific psychotherapies is 36%, showing how tough these paths can be. Many feel stuck, unable to find lasting peace.
This is where ketamine therapy offers a groundbreaking new possibility. It has been found to relieve PTSD symptoms in some cases within hours, unlike other medications that can take weeks. This rapid effect opens a unique window for healing and growth.
I'm Bambi Rattner, PsyD, and I've spent decades helping people heal, constantly seeking more effective ways. My work in EMDR and Progressive Counting, combined with intensive trauma retreats, has shown me the power of deep, lasting change, preparing me to understand the transformative potential of ketamine for trauma therapy. This guide will explore how this innovative treatment works and how it can help you reclaim your life.
Understanding Ketamine and Its Role in Healing Trauma
You might know ketamine as that medication used in operating rooms and emergency departments. It's been around since 1970, when the FDA first approved it as an anesthetic. But here's where things get interesting – over the past few decades, researchers have finded something remarkable about this old drug. When used in much smaller doses than what's needed for surgery, ketamine has shown incredible promise for mental health conditions, especially trauma.
Ketamine for trauma therapy works very differently from its use in surgery. Instead of putting you completely under, these lower "sub-anesthetic" doses create what doctors call a dissociative experience. This might sound scary, but it's actually one of the reasons ketamine can be so helpful for trauma survivors.
Think of it this way: when you're in this gentle dissociative state, you can step back from your usual thought patterns and emotions. It's like being able to observe your traumatic memories from a safe distance, rather than being overwhelmed by them. Many people describe feeling temporarily detached from their body or having an almost dream-like experience that can last anywhere from 40 minutes to a few hours.
This isn't the same as recreational use of ketamine, which can be dangerous and unpredictable. In a therapeutic setting, everything is carefully monitored and controlled to create the most healing experience possible.
How Ketamine Works in the Brain
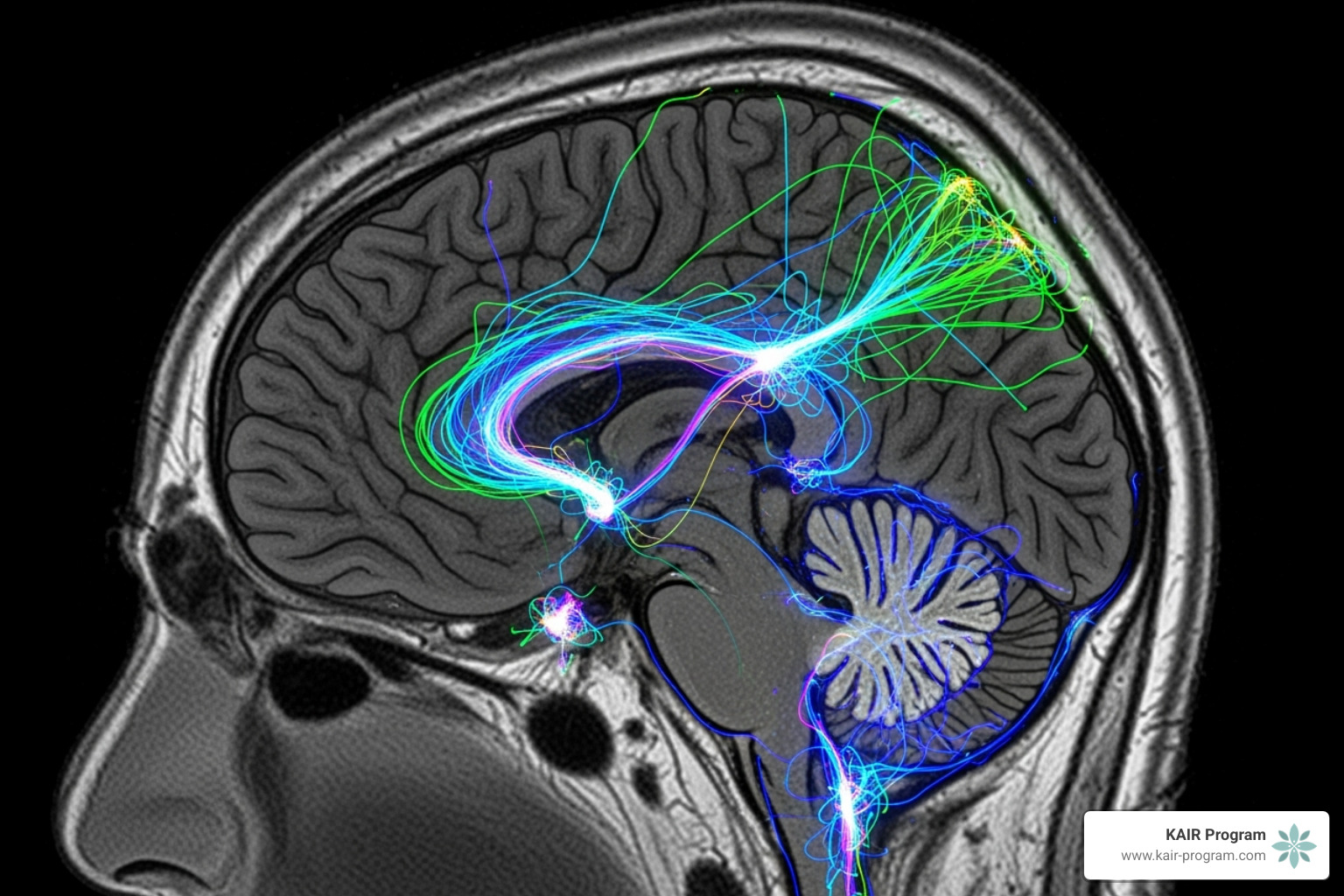
The science behind ketamine's healing power is truly fascinating. Deep inside your brain, there's a complex communication system that uses a chemical messenger called glutamate. Think of glutamate as your brain's main "on" switch – it's essential for learning and forming memories.
Ketamine works by temporarily blocking something called NMDA receptors, which are like the receiving stations for glutamate messages. When ketamine blocks these receptors, it starts a chain reaction that leads to some pretty amazing changes in your brain.
One of the most important things that happens is a rapid increase in Brain-Derived Neurotrophic Factor (BDNF). If you've never heard of BDNF, think of it as fertilizer for your brain cells. It helps create new connections between neurons, a process called synaptogenesis. This is all part of something called neuroplasticity – your brain's incredible ability to rewire itself and form new pathways.
For trauma survivors, this is huge. Trauma can create rigid patterns in the brain, like well-worn paths that always lead to the same places – fear, avoidance, or emotional numbness. Ketamine essentially helps "reboot" these stuck patterns, making your brain more flexible and open to new ways of thinking and feeling.
You can learn more about the detailed neurobiological mechanism of ketamine if you're interested in diving deeper into the science.
From Anesthetic to a Guide of Hope for Trauma Survivors
This brain-rebooting ability makes ketamine particularly powerful for conditions like Post-Traumatic Stress Disorder (PTSD) and Complex PTSD (C-PTSD). C-PTSD often develops from prolonged or repeated trauma, like childhood abuse or being in an abusive relationship for years.
Ketamine has also shown promise for Treatment-Resistant Depression (TRD), comorbid anxiety, and even suicidal ideation. These conditions often involve brain pathways that seem stuck in harmful patterns, resistant to change through traditional treatments alone.
But here's what makes ketamine truly special: its rapid-acting effects. While traditional antidepressants can take weeks or even months to show improvement, many people experience symptom relief within hours of their first ketamine session. Imagine struggling with severe depression or PTSD symptoms for years, then feeling genuine relief in just a few hours – it can feel nothing short of miraculous.
This quick response isn't just about feeling better faster. It creates what therapists call a "window of opportunity" – a time when your brain is more flexible and ready for the deeper work of healing. For people dealing with severe emotional pain or thoughts of suicide, this rapid relief can be life-changing, providing immediate hope and reducing dangerous symptoms while longer-term healing begins.
The Science-Backed Efficacy of Ketamine for Trauma Therapy
When you're struggling with trauma, you want to know that any treatment you consider actually works. The good news is that ketamine for trauma therapy has solid science behind it, with research showing impressive results for rapid symptom reduction.
What makes ketamine particularly exciting is how quickly it can work. While traditional medications might take weeks to show benefits, ketamine can provide relief within hours. This rapid response isn't just temporary relief either – clinical trials show that the effects can last weeks, especially when combined with psychotherapy integration.
The research findings paint a hopeful picture. Studies consistently show that ketamine helps a significant number of people who haven't found relief elsewhere. The durability of these effects becomes even stronger when patients engage in ongoing therapy work to integrate their experiences and build on their progress.
Breaking Down the Research: How Effective is Ketamine for PTSD?
Let's look at the actual numbers, because they're pretty remarkable. In one significant study, 67% of patients who received ketamine achieved what researchers call a "treatment response" – meaning their PTSD symptoms dropped by at least 30%. Compare that to only 20% in the placebo group, and you can see why researchers are excited.
But the benefits go beyond just symptom scores. When we look at real-world impact, the changes are dramatic. People with both treatment-resistant depression and PTSD who received ketamine treatment had 65% fewer psychiatric hospital admissions and spent 70% fewer days in the hospital overall. That's not just better mental health – that's getting your life back.
The relief doesn't disappear overnight either. Patients who responded well to ketamine stayed improved for a median of 4 weeks after completing their initial series of six infusions. This gives you time to work with your therapist to build on the progress and develop new coping skills.
Across multiple studies, about 75% of patients find relief through ketamine therapy. A comprehensive meta-analysis on ketamine for PTSD backs up these individual study results, showing consistent benefits across different research groups and settings.
Beyond PTSD: Addressing Comorbid Conditions
Here's something important to understand: trauma rarely travels alone. If you're dealing with PTSD, there's a good chance you're also struggling with depression, anxiety, or other mental health challenges. About half of people with PTSD also have major depression, which can make treatment more complex.
This is where ketamine for trauma therapy really shines. Instead of needing separate treatments for each condition, ketamine can address multiple issues at once. In a study on comorbid TRD and PTSD, the results were stunning: 80% of patients achieved PTSD remission and 93.3% had a positive response for their treatment-resistant depression.
This holistic healing approach means you're not just managing symptoms – you're addressing the root of interconnected mental health challenges. When trauma, depression, and anxiety are all improved together, the overall quality of life improvements can be truly transformative.
The research shows that ketamine doesn't just treat one piece of the puzzle. It helps create the neuroplasticity needed for your brain to heal from multiple trauma-related conditions at once, giving you a real chance at comprehensive recovery.
The Ketamine-Assisted Psychotherapy (KAP) Process Explained

Here's the truth about ketamine for trauma therapy: it's not just about taking a medication and hoping for the best. Real healing happens when we combine ketamine's unique effects with thoughtful, skilled therapy support. This is what we call Ketamine-Assisted Psychotherapy, or KAP for short.
Think of KAP as a carefully orchestrated dance between medicine and therapy. The ketamine opens doors in your mind that might have been locked for years, but you need a skilled guide to help you walk through those doors safely. That's where the therapeutic relationship becomes absolutely crucial.
We follow what therapists call the "set and setting" approach. Your mindset going into the experience and the environment around you can make all the difference. When you feel safe with your therapist and clear about your goals, the ketamine can do its best work. This isn't a one-time event either – it's a journey with three distinct phases that work together to create lasting change.
Step 1: Preparation and Setting Intentions
Before you ever experience ketamine, we spend significant time getting to know you and your story. This begins with a thorough initial consultation where we dive deep into your history, your struggles, and what you're hoping to achieve.
The medical screening is essential because ketamine affects your body as well as your mind. We need to make sure your heart, blood pressure, and overall physical health can handle the treatment safely. Equally important is the psychological evaluation, where we explore your trauma history, current symptoms, and any previous treatment experiences.
But here's what makes this different from a typical doctor's visit: we're also building rapport and trust. You'll be in a vulnerable state during ketamine sessions, so feeling genuinely safe with your therapeutic team isn't just nice to have – it's absolutely necessary for healing to occur.
Together, we'll work on defining your treatment goals and setting clear intentions for your healing journey. What would your life look like if you could process your trauma without being overwhelmed by it? How would you feel if those intrusive memories lost their power over you? These conversations help create a roadmap for your sessions and ensure we're working toward outcomes that truly matter to you.
Step 2: The Ketamine Experience
When it's time for your ketamine session, you'll be in a supervised clinical setting with continuous medical monitoring. Safety is our top priority, and you'll never be alone during this experience.
Ketamine can be given through several methods. Intravenous (IV) infusion delivers the medication directly into your bloodstream and typically lasts about 40 minutes. Intramuscular (IM) injection is another option, while oral lozenges create a longer experience that can last up to 3 hours. We'll discuss which method feels right for your specific needs and comfort level.
During the session, you'll enter what we call the dissociative state. This might sound scary, but many people find it surprisingly peaceful. You might feel like you're floating above your body or watching your thoughts from a distance. Time might seem to slow down or speed up. Colors might seem more vivid, or you might have insights that feel profound and meaningful.
Here's the remarkable part: in this state, you can often process trauma with reduced fear. Those memories that usually trigger panic or overwhelming emotions become more manageable. It's like being able to look at a scary movie from behind a protective shield – you can see what's happening, but it can't hurt you in the same way.
Step 3: Integration: The Key to Lasting Change in Ketamine for Trauma Therapy
This is where the real magic happens. The ketamine experience itself is just the beginning – post-session psychotherapy is where you transform insights into lasting change.
In the days and weeks following your ketamine session, your brain is in what we call "the window of neuroplasticity." Think of it like fresh concrete – it's still moldable and ready to form new, healthier patterns. This is the perfect time to work with your therapist on making sense of the experience and connecting insights to daily life.
Maybe during your session, you realized that your hypervigilance stems from feeling unsafe as a child. Or perhaps you experienced a profound sense of self-compassion for the first time. These insights are valuable, but they need to be woven into your everyday life to create real change.
Your therapist will help you develop new coping mechanisms based on what you learned during the ketamine experience. Together, you'll work on rewriting the trauma narrative – not changing what happened, but changing how those experiences affect you now.
This integration work is what transforms a powerful but temporary experience into genuine, lasting healing. It's the difference between having a beautiful dream and waking up to find your life has actually changed for the better.
Is Ketamine Therapy Safe? Navigating Risks and Side Effects
When you're considering ketamine for trauma therapy, it's natural to wonder about safety. The good news is that when administered in a controlled, clinical environment under the supervision of experienced medical professionals, ketamine therapy is considered safe for most individuals.
The key difference lies in how it's used. Therapeutic ketamine is worlds apart from recreational use - the dosages, administration methods, and monitoring are entirely different. Think of it like the difference between a carefully prescribed medication and something used without medical guidance. That's why comprehensive medical screening beforehand is so essential to ensure your suitability for treatment.
Potential Short-Term Side Effects
Like any medication, ketamine can have side effects, though they're typically temporary and well-managed within our clinical setting. You might experience nausea, which we often manage with anti-nausea medication. Dizziness is another common effect that's temporary, usually resolving shortly after your session.
The dissociation - that "out-of-body" or detached feeling - is actually a key therapeutic effect, though it can feel unusual if you've never experienced it before. We'll prepare you for this sensation so you know what to expect.
During your session, you might notice increased blood pressure and heart rate. These vital signs are closely monitored throughout, and we have interventions available if needed. Some people experience mild, temporary confusion or even brief anxiety. While ketamine aims to reduce anxiety overall, some individuals may feel temporary anxiety during or immediately after the session.
All these effects are closely monitored by our medical team and generally resolve within minutes to a few hours after your session. We make sure you're fully recovered and stable before you leave our care.
Who is a Good Candidate for Ketamine Therapy?
Ketamine for trauma therapy isn't right for everyone, but it can be profoundly effective for the right individuals. You might be a good candidate if you're an adult with diagnosed PTSD or Complex PTSD.
This treatment particularly shines for those with treatment-resistant conditions - meaning you haven't found adequate relief from traditional therapies or medications like SSRIs. If you've tried multiple approaches without success, ketamine might offer the breakthrough you've been seeking.
Equally important is being motivated for psychotherapy and committed to the integration process. The combination of ketamine and therapy is where the most significant and lasting changes often occur, so your willingness to engage in this work is crucial.
Who Should Avoid Ketamine for Trauma Therapy?
While safe for many, certain conditions may exclude individuals from ketamine therapy due to potential risks. It's crucial to be completely honest about your medical history during our screening process.
We typically can't proceed if you have a history of psychosis, such as schizophrenia, or active bipolar mania. Uncontrolled hypertension or severe cardiovascular disease also present risks we can't safely manage. If you have a history of active substance use disorder, this can complicate treatment and increase risks.
Pregnancy or breastfeeding are also contraindications, as are certain neurological conditions that might be worsened by ketamine.
Our thorough medical and psychological evaluation process is designed to identify any potential contraindications. This isn't about excluding people - it's about ensuring your safety and optimizing the potential for therapeutic benefit. We want to make sure ketamine therapy is not just effective for you, but completely safe as well.
Frequently Asked Questions about Ketamine for Trauma Therapy
It's completely natural to have questions when exploring a new path to healing. We're here to provide clear, compassionate answers to some of the most common inquiries about ketamine for trauma therapy.
What does a ketamine session feel like?
This is one of the most frequently asked questions, and for good reason! The experience of a ketamine session is truly unique for everyone, and it can even be different each time you have a session. Many describe it as entering a gentle, dream-like state. You might notice your perceptions of time and space shift, feeling a sense of detachment from your everyday thoughts and worries.
Some people experience a profound emotional release, while others feel a comforting sense of detachment from their physical body. You might even feel a deep sense of connection or unity with something larger than yourself. Some report vivid imagery or new insights that can be quite profound. It's a very personal journey into a non-ordinary state of consciousness that can open doors for introspection and deep healing. Rest assured, our team will be there to guide you, answer any questions, and support you every step of the way.
How many sessions will I need?
There's no single answer to this, as your healing journey is as unique as you are. The number of sessions you'll need for ketamine for trauma therapy depends on several factors: your individual needs, how severe your condition is, and how your body and mind respond to the treatment.
Typically, a course of treatment begins with a series of initial sessions. For example, many people start with around six infusions given over a period of two to three weeks. After this initial phase, some individuals find that "booster" or maintenance sessions are helpful, perhaps every few weeks or months, to maintain their progress. Our main goal is to help you achieve lasting relief and truly integrate the powerful insights you gain into your daily life. We'll continuously assess your progress and work with you to create a personalized treatment plan that perfectly fits your evolving needs.
Is ketamine therapy for trauma covered by insurance?
This is a very important and common question for many considering ketamine for trauma therapy. Insurance coverage can vary quite a bit. Because ketamine's use for PTSD is often considered "off-label" – meaning it's not specifically FDA-approved for this exact condition, even though it's a legal and widely practiced treatment – many insurance providers don't yet cover the full cost of the ketamine administration itself.
However, there's good news! Parts of your treatment, like the important preparatory and integration psychotherapy sessions, might be covered by your health insurance plan. This depends on your specific policy and benefits. We know that cost can sometimes feel like a barrier to getting the care you need. We always recommend reaching out directly to your insurance provider to understand your specific benefits. Additionally, many clinics, including ours, offer different financing options or payment plans to help make this life-changing treatment more accessible.
The Future of Trauma Treatment and How to Get Started

The landscape of mental healthcare is undergoing a significant change, and ketamine for trauma therapy is at the forefront of this exciting shift. Ongoing research and clinical trials are continually expanding our understanding of ketamine's mechanisms and optimal applications for PTSD and related conditions. Researchers are working to standardize protocols, exploring different administration methods, and investigating which psychotherapy models best complement ketamine's effects. You can find more information on current clinical trials for ketamine and PTSD.
This represents a paradigm shift in how we approach mental health, moving towards more rapid, profound, and holistic healing. For too long, individuals with treatment-resistant trauma have felt stuck, but ketamine offers a guide of hope, providing a pathway to relief that was once unimaginable.
Taking the first step towards healing can be daunting, but it's a powerful act of self-compassion. At KAIR Program, we are dedicated to guiding you through this journey. Our unique approach combines the transformative potential of ketamine with intensive, trauma-focused retreats. We believe that by integrating the neurobiological changes facilitated by ketamine with deep, expert-led psychotherapy, we can help you achieve rapid, lasting healing from the wounds of trauma.
If you're ready to explore how ketamine-assisted therapy can help you reclaim your life and move towards a future filled with hope and well-being, we invite you to connect with us. Learn more about our ketamine-assisted retreats for trauma and begin your path to profound healing.
