Obsessive Thoughts Meet Ketamine Therapy—A Promising Pair?
When Traditional OCD Treatment Isn't Enough

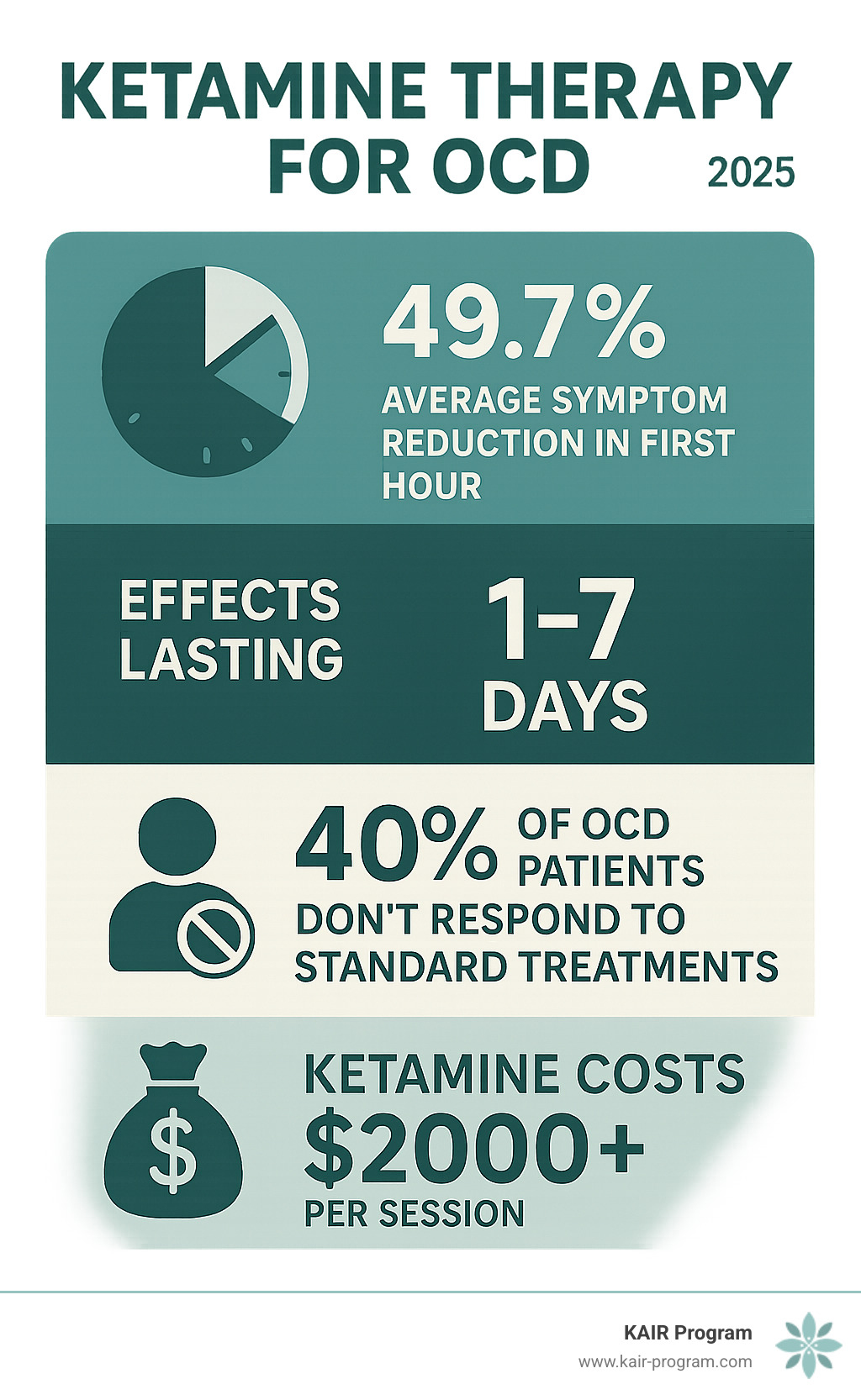
Ketamine therapy for OCD represents a breakthrough approach for people who haven't found relief through conventional treatments. While research is still emerging, studies show that ketamine can reduce OCD symptoms by approximately 49.7% within the first hour of treatment - though these effects are typically short-lived, lasting about one to seven days.
Quick Facts About Ketamine for OCD:
- Not FDA-approved specifically for OCD (used off-label)
- Rapid onset - effects can begin within hours, not weeks
- Targets glutamate system instead of serotonin like traditional medications
- Temporary relief - symptoms often return within 3-7 days without maintenance
- Research status - promising but limited studies available
- Best for treatment-resistant cases with proper medical supervision
The reality is stark: approximately 40% of people with OCD find standard treatments ineffective. For those stuck in the exhausting cycle of obsessions and compulsions despite years of therapy and medication, ketamine offers a different path forward.
Geuris "Jerry" Rivas captured this hope perfectly after participating in the first clinical trial for ketamine in OCD: "I tried to have OCD thoughts, but I couldn't. I feel as if the weight of OCD has been lifted."
While ketamine isn't a cure-all, it's opening new possibilities for people who've run out of options. The treatment works by targeting the brain's glutamate system rather than serotonin, potentially "resetting" stuck neural patterns that drive obsessive thoughts and compulsive behaviors.
I'm Dr. Bambi Rattner, a licensed psychologist who has worked extensively with trauma and anxiety disorders, including treatment-resistant conditions where ketamine therapy for OCD shows particular promise. Through my experience with intensive therapy models and ketamine-assisted treatment, I've seen how this approach can create breakthrough moments for people who've struggled for years with traditional methods.
Understanding Ketamine and Its Novel Approach to OCD
Ketamine has quite a story. Back in the 1960s, doctors developed it as an anesthetic - something to keep patients comfortable during surgery. For decades, it did exactly that job in operating rooms around the world. But ketamine had some interesting properties that set it apart from other anesthetics.
Unlike medications that knock you out completely, ketamine creates what doctors call dissociative effects. Patients might feel disconnected from their body or surroundings, but they don't necessarily lose consciousness entirely. This unique quality would later become crucial for its mental health applications.
Here's where things get really interesting: ketamine therapy for OCD works nothing like traditional treatments. While almost every antidepressant developed in the past 60 years focuses on serotonin or similar neurotransmitters, ketamine completely ignores the serotonin system. Instead, it targets something entirely different - the brain's glutamate system.
How Ketamine Works in the Brain
Think of your brain as having two main chemical messaging systems. Most people have heard of serotonin - that's the "feel good" neurotransmitter that SSRIs try to boost. But there's another system that's actually much more active: glutamate.
Glutamate is your brain's primary excitatory neurotransmitter. It's involved in nearly every brain function you can think of - learning, memory, and most importantly for OCD, the brain's ability to change and adapt (what scientists call neuroplasticity).
Ketamine works as an NMDA receptor antagonist. In plain English, this means it temporarily blocks certain receptors that glutamate normally activates. When this happens, something remarkable occurs: the brain starts producing more brain-derived neurotrophic factor (BDNF).
BDNF acts like fertilizer for your neurons. It helps brain cells grow new connections and form fresh pathways. This process is called synaptic plasticity - essentially your brain's ability to rewire itself. Scientific research on glutamate's role shows just how fundamental this neurotransmitter system is to brain function.
The result? Ketamine may give your brain a chance to break free from stuck patterns and create new, healthier neural pathways. It's like hitting a reset button on circuits that have been running the same problematic program over and over.
Why This Mechanism Matters for OCD
If you've tried traditional OCD treatments, you know the frustration. SSRIs can take 8-12 weeks to show any effect - if they work at all. That's a long time to wait when you're struggling with intrusive thoughts and compulsions every day.
Even worse, these serotonin-focused medications simply don't work for everyone. This creates what researchers call an "effectiveness gap" - a crucial period where people continue suffering while hoping their medication will eventually kick in.
The glutamate dysfunction in OCD offers a completely different target for treatment. Research suggests that OCD involves specific brain circuits getting "stuck" in repetitive patterns. These circuits connect areas like the orbitofrontal cortex, anterior cingulate cortex, and striatum - regions involved in decision-making, error detection, and movement control.
When these circuits malfunction, it's like having a broken record player in your brain. The same thoughts and behaviors keep repeating, no matter how much you want them to stop.
By targeting the glutamate system instead of serotonin, ketamine offers potential for rapid change. Rather than slowly building up neurotransmitter levels over weeks, ketamine can potentially disrupt stuck neural patterns within hours. This creates a window of opportunity where the brain might be more flexible and able to form new, healthier connections.
This is why ketamine therapy for OCD represents such a paradigm shift. We're not just treating symptoms - we're potentially giving the brain the tools it needs to rewire itself and break free from the cycles that drive obsessive-compulsive behaviors.
The Evidence: What Research Says About Ketamine for OCD
The research on ketamine therapy for OCD is still in its early stages, but the results are encouraging. Most studies use the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), the gold standard for measuring OCD severity, to track improvements.
Key Findings from Clinical Studies
The most striking finding is the speed of ketamine's effects. In studies examining rapid anti-obsessive treatments, researchers found that OCD scores decline by approximately 49.7% during the first hour following intravenous ketamine administration. This is remarkable compared to traditional treatments that take weeks or months to show benefits.
However, there's a catch - these effects aren't sustained. Eight studies revealed rapid anti-obsessive effects, with five showing statistical significance, but the benefits typically reverse within seven days. Obsessions and compulsions often begin returning within three hours post-administration.
A 2013 proof-of-concept trial randomized 15 patients with OCD to receive either ketamine or placebo. The results were encouraging: diminished symptoms lasted throughout the following week in half of the patients who received ketamine. One participant described the experience as "right out of a movie."
Currently, a five-year trial is underway, aiming to follow 90 OCD patients for up to six months after they receive ketamine or an alternative treatment. This larger study will help us better understand ketamine's long-term potential and optimal dosing strategies.
The Potential of Ketamine Therapy for OCD in Severe Cases
Perhaps the most compelling evidence comes from case reports of severe, treatment-resistant OCD. In one remarkable case from Bangladesh, a 24-year-old male with extremely severe OCD (Y-BOCS score of 40) and severe suicidal ideation experienced dramatic improvement after three weekly ketamine infusions.
His Y-BOCS score dropped from 40 (extremely severe) to 4 (subclinical) after multiple infusions, with improvement sustained for 12 weeks. Even more importantly, his suicidal ideation - which had led to a suicide attempt - decreased from severe to minimal levels.
This case is particularly significant because it demonstrates ketamine's potential for the most challenging OCD cases. OCD sufferers have a 10 times higher rate of death by suicide than the general population, making rapid intervention crucial. Ketamine's ability to quickly decrease suicidal thinking within 2-24 hours after a single infusion could be life-saving for some individuals.
The Ketamine Treatment Journey: Process, Safety, and Candidacy

If you're considering ketamine therapy for OCD, you're probably wondering what the actual experience looks like. It's quite different from swallowing a pill each morning - think of it more like a carefully orchestrated medical procedure that requires your full attention and commitment.
How Ketamine is Administered for OCD
The treatment happens in a clinical setting that looks more like a comfortable medical office than a hospital. You'll receive ketamine through an intravenous (IV) infusion while relaxing in a reclining chair, with medical professionals monitoring you throughout the entire process.
Ketamine is not FDA-approved specifically for OCD - doctors use it "off-label" based on emerging research. This means your insurance likely won't cover it, and you'll need to work with a provider experienced in this type of treatment.
A typical treatment course unfolds in two phases. During the induction phase, you might receive infusions once or twice weekly for several weeks. If you respond well, you may enter a maintenance phase with less frequent treatments to help sustain the benefits.
Each session lasts about 40-60 minutes. The typical dose is around 0.5 mg/kg, diluted in normal saline and delivered slowly through your IV. You'll remain conscious throughout, though you may experience what doctors call "dissociative effects" - a temporary feeling of being detached from your body or surroundings.
Potential Risks and Side Effects
Let's be honest about what you might experience. Ketamine has been used safely in medical settings for over 50 years, but it's not a walk in the park. Most people experience some side effects during or shortly after treatment.
Dissociation is the most common effect - you might feel like you're watching yourself from outside your body or that reality seems dreamlike. While this can feel unsettling, it's temporary and usually resolves within an hour. Some people actually find this experience helpful for gaining new perspectives on their thoughts and feelings.
Nausea affects many patients, though it typically passes quickly. Your treatment team can provide medications to help manage this if needed. Dizziness is another common effect that makes it important to have someone drive you home after treatment.
Increased blood pressure is why continuous monitoring is essential. Your heart rate and blood pressure will be checked regularly throughout the infusion. This is also why certain medical conditions make ketamine unsuitable for some people.
The DEA information on ketamine risks emphasizes concerns about potential for misuse and psychological dependence with long-term use. This is why proper medical supervision isn't just recommended - it's absolutely crucial.
Most side effects fade within an hour or two after treatment. The clinical setting provides safety and support, with trained healthcare providers ready to manage any adverse reactions that might occur.
Who is a Good Candidate for This Therapy?
Ketamine therapy for OCD isn't a first-line treatment - it's typically reserved for people who've already tried multiple approaches without success. If you've been through several SSRIs, spent months in cognitive-behavioral therapy, tried Exposure and Response Prevention, and still struggle with severe symptoms, you might be a good candidate.
People with co-occurring depression often respond particularly well, since ketamine has stronger evidence for treating depression and can address both conditions simultaneously. If you're dealing with suicidal thoughts alongside your OCD, the rapid anti-suicidal effects of ketamine might make treatment more urgent and potentially life-saving.
However, certain conditions make ketamine unsuitable or dangerous. Who should avoid ketamine includes people with psychosis (ketamine can worsen these symptoms), uncontrolled cardiovascular disease (the treatment affects blood pressure and heart rate), severe liver disease (ketamine is processed by the liver), and pregnancy (safety hasn't been established).
The screening process is thorough because safety comes first. Your medical team will review your complete medical history, current medications, and psychiatric conditions. They'll also assess whether you have adequate support at home and realistic expectations about the treatment process.
Comprehensive medical screening isn't just a formality - it's essential for determining whether ketamine is both safe and likely to be helpful for your specific situation.
How Ketamine Therapy Differs from Traditional OCD Approaches
| Factor | Ketamine Therapy | Traditional Approaches |
|---|---|---|
| Onset of Action | Hours to days | Weeks to months |
| Duration of Effects | Days to weeks | Ongoing with continued use |
| Mechanism | Glutamate system (NMDA receptors) | Serotonin system |
| Treatment Setting | Clinical infusion center | Home-based medication, therapy office |
The differences between ketamine therapy for OCD and traditional treatments are striking. When you've been waiting months for an SSRI to maybe work, the idea of feeling relief within hours can seem almost too good to be true.
Ketamine's Unique Benefits
Speed is ketamine's superpower. While most people wait 8-12 weeks to see if their antidepressant will help their OCD, ketamine can provide noticeable symptom relief within the first few hours. For someone who's been trapped in obsessive thoughts and compulsive behaviors for years, this rapid change can feel miraculous.
The fact that ketamine targets the glutamate system instead of serotonin is equally game-changing. If you've tried multiple SSRIs without success, ketamine offers a completely different approach. It's like trying a different key when the first one won't turn the lock.
Many people also find ketamine's side effect profile more manageable than long-term SSRI use. While dissociation and temporary nausea aren't pleasant, they're short-lived compared to the ongoing sexual dysfunction, weight gain, or emotional numbness that can come with traditional medications.
But here's the honest truth: sustainability is ketamine's biggest challenge. Traditional treatments, when they work, can provide steady relief as long as you continue taking them. Ketamine's effects are more like a brief vacation from your symptoms - powerful but temporary.
Integrating Ketamine with Therapeutic Support
This is where the magic really happens. Ketamine doesn't just reduce symptoms temporarily - it creates what we call a window of neuroplasticity. Your brain becomes more flexible and open to change, like clay that's been warmed up and is ready to be reshaped.
This is the perfect time for intensive therapy work. At KAIR Program, we've seen how combining ketamine with trauma-focused therapy during our intensive retreats allows people to make breakthrough progress while their brains are in this improved state.
Think of it this way: ketamine opens the door that's been locked for years, but you still need to walk through it. The combination of pharmacological and behavioral support gives you the best chance of building new coping skills and creating lasting change.
Without proper therapeutic support, ketamine becomes just a temporary Band-Aid. But when you use that window of increased brain plasticity for deep therapeutic work, you can create patterns and insights that last long after the ketamine has worn off.
Financial and Accessibility Considerations
Let's be honest - ketamine therapy for OCD isn't cheap. The reality is that treatment can cost $2,000 or more per session, and since it's not FDA-approved specifically for OCD, most insurance companies won't cover it. You'll likely be paying out of pocket for most, if not all, of your treatment.
Even when insurance companies do offer partial coverage, they typically require extensive documentation showing that you've tried and failed multiple conventional treatments first. This means jumping through hoops to prove that standard medications and therapy haven't worked for you.
The financial burden can feel overwhelming, especially when you're already struggling with the exhausting cycle of OCD symptoms. Many people find themselves weighing the potential benefits against the significant cost, particularly since ketamine's effects are often temporary and require repeated treatments to maintain.
Finding a qualified provider adds another layer of complexity. Qualified providers are often concentrated in urban areas, which can create challenges for those in more rural locations. If you live in a smaller city or rural area, you might need to travel considerable distances for treatment.
Not all ketamine providers have experience with OCD specifically. While ketamine is ketamine, the nuances of treating OCD versus depression can be different. You'll want to research clinics that specialize in ketamine therapy, check their credentials, and ask about their specific experience with OCD patients.
The off-label status creates additional challenges beyond just cost. While off-label prescribing is perfectly legal and common in medicine, it means there are fewer standardized protocols. Different clinics might have varying approaches to dosing, frequency, and monitoring.
This lack of standardization means you'll need to be an active advocate for your own care. Work closely with your healthcare team to understand the treatment plan, ask questions about their experience, and make sure you're comfortable with their approach before beginning treatment.
At KAIR Program, we understand these accessibility challenges. Our intensive retreat format allows people to receive comprehensive treatment in a concentrated timeframe, potentially reducing the overall number of sessions needed while maximizing the therapeutic benefit during ketamine's window of improved neuroplasticity.
Conclusion: A Promising but Cautious Path Forward
Ketamine therapy for OCD represents one of the most exciting developments in mental health treatment in decades. For people who've tried everything else without success, the ability to experience significant symptom relief within hours - not months - can feel nothing short of miraculous.
But let's be honest about what we know and what we don't. The effects are rapid but they're also temporary, typically lasting only days to weeks. This isn't a magic cure, and it's definitely not something to try before proven treatments like Exposure and Response Prevention therapy or SSRIs.
The real breakthrough happens when we stop thinking of ketamine as a standalone treatment and start seeing it as a powerful tool that can improve other therapies. Think of it this way: if your brain has been stuck in the same patterns for years, ketamine creates a window where those patterns become more flexible and changeable.
That's exactly why we developed our approach at KAIR Program. We don't just give people ketamine and send them home. We combine it with intensive, trauma-focused therapy in a retreat setting where people can dive deep into healing work while their brains are in this improved state of neuroplasticity.
The future of OCD treatment isn't about choosing between traditional therapy and ketamine - it's about using them together strategically. As research continues and we learn more about optimal protocols, we expect to see even better outcomes for people with treatment-resistant conditions.
If you're considering this path, the most important thing is finding providers who understand both the incredible potential and the real limitations of ketamine therapy. You want someone who can integrate it thoughtfully with comprehensive therapeutic support, not just administer it in isolation.
The journey with OCD can feel impossibly long and frustrating. But treatments like ketamine therapy for OCD are opening doors that seemed permanently locked. While we're still learning how to use this powerful tool most effectively, the early results offer genuine hope for people who've been waiting far too long for relief.
Learn more about our ketamine-assisted retreats and how we're pioneering this integrated approach to healing. Sometimes the breakthrough you've been searching for is closer than you think.

