Unlocking the Mind with Psychedelic Mental Health Treatments
A New Dawn for Mental Wellness
Psychedelic mental health represents a approach to treating conditions that have resisted traditional therapies for decades. This emerging field combines powerful mind-altering substances with guided psychotherapy to create profound healing experiences.
Key aspects of psychedelic mental health treatment include:
- Rapid results: Significant improvement in depression within 24 hours of ketamine treatment.
- Treatment-resistant conditions: Hope for PTSD, depression, and anxiety that haven't responded to standard care.
- Neuroplasticity: Promotes brain rewiring for lasting change.
- Guided therapy: Always conducted with trained professionals in controlled settings.
- Integration focus: Emphasizes processing insights for long-term healing.
The need for new options is urgent. Hundreds of millions of people worldwide live with depression and anxiety, yet traditional treatments fail a significant portion of them. For instance, 40-60% of people with PTSD don't respond to SSRIs, and about one-third of those with major depression face treatment-resistant symptoms. Many cycle through medications without finding relief, leading them to seek alternatives.
The science backs up this shift. Clinical trials show single doses of psilocybin can produce "rapid, robust, and sustained" reductions in depression. MDMA-assisted therapy has shown remarkable success for severe PTSD, with over 71% of participants no longer meeting diagnostic criteria.
I'm Dr. Bambi Rattner, and I've spent decades in mental health treatment. My journey led me from traditional practice to intensive trauma therapy and now to the promising field of psychedelic mental health. Here, I've seen clients achieve breakthrough healing that other methods couldn't provide.
The Resurgence of Psychedelics: From Counterculture to Clinical Trials
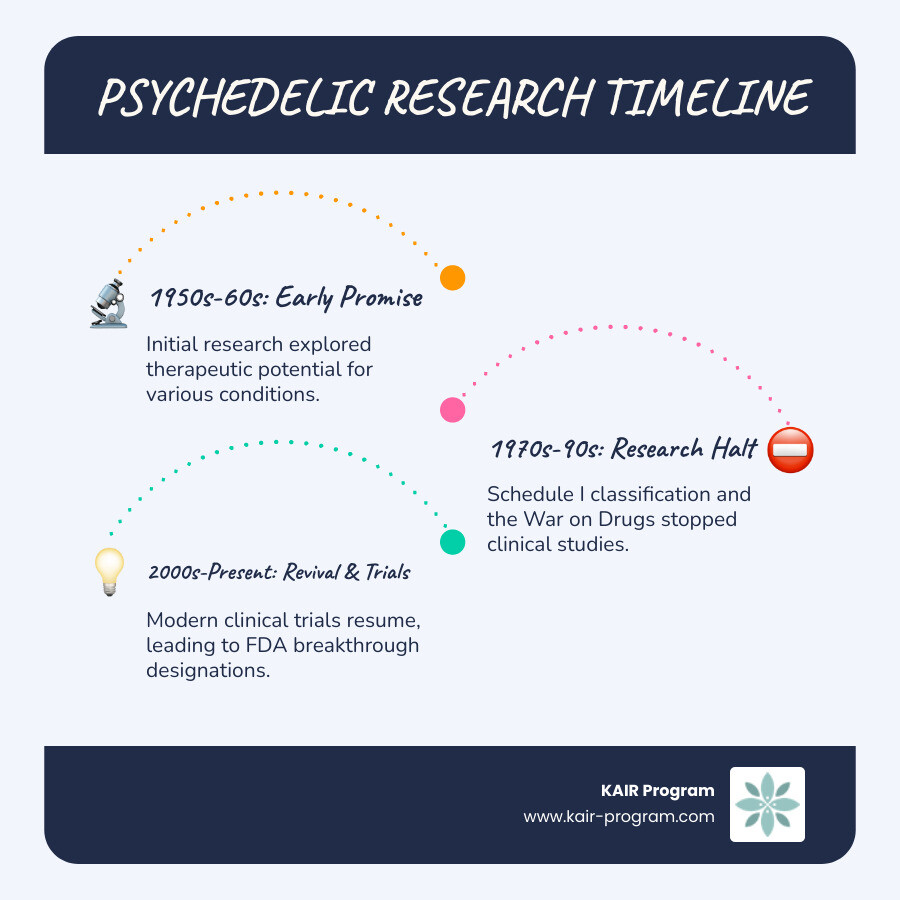
The journey of psychedelic mental health treatment has been dramatic. In the 1950s, researchers were excited about LSD and psilocybin, studying them for everything from depression to addiction with promising results. These were considered serious psychiatric tools, not street drugs.

However, the cultural upheaval of the 1960s and the subsequent War on Drugs led to a severe backlash. These compounds were classified as Schedule I substances, deemed to have "no currently accepted medical use," which halted research for nearly three decades. Around 2000, pioneering researchers at institutions like Johns Hopkins began to revisit these substances, sparking the modern "psychedelic renaissance."
This resurgence is driven by a critical need for better treatments. Current therapies are failing millions. About one-third of people with major depression have treatment-resistant symptoms, and 40-60% of PTSD patients don't respond to standard care. People are stuck cycling through medications with minimal relief. Psychedelic therapies offer a different path: rapid, robust, and sustained effects, often after just a single guided session.
The legal and regulatory landscape is also shifting rapidly. We're seeing decriminalization movements and state-level legalization for therapeutic use, such as Oregon's Psilocybin Services Act. At the federal level, the FDA has granted Breakthrough Therapy designations to both psilocybin and MDMA for depression and PTSD, respectively. This designation fast-tracks the development of treatments that show substantial improvement over existing options.
The FDA's willingness to consider approval and the return of federal research funding signal a major change. We are moving from viewing these compounds as dangerous drugs to recognizing them as potentially life-saving medicines. The momentum toward medical legalization is undeniable.
How Psychedelics Rewire the Brain for Healing
What makes psychedelic mental health treatments so different is how they change the brain. Instead of just managing symptoms, they can fundamentally rewire neural pathways, breaking rigid patterns of depression, anxiety, and trauma.
Think of a brain stuck in depression as having deeply worn, negative thought-grooves. Psychedelics shake up these rigid pathways, allowing new, healthier connections to form. They do this by targeting the brain's serotonin system and quieting the Default Mode Network (DMN)—the part of the brain responsible for self-referential thinking and rumination. When the DMN is less active, people can experience ego dissolution, a temporary softening of the self that allows for new perspectives. This state of flexible brain activity, or increased brain entropy, is highly therapeutic and often linked to profound mystical experiences that correlate with positive outcomes.
The Neurological Magic: Neuroplasticity and Brain Connectivity
The core mechanism is neuroplasticity—the brain's ability to form new connections. Psychedelics act like fertilizer for neurons, promoting rapid growth through several processes:
- Synaptogenesis: The formation of new synapses (connections) between brain cells.
- Dendritic growth: The growth of new branches on neurons to communicate with others.
These processes are fueled by a boost in Brain-Derived Neurotrophic Factor (BDNF) and activation of the mTOR pathway, both crucial for cellular growth. Scientific research on 5-HT2A receptor activation confirms that these compounds trigger growth-promoting signals in neurons. The result is increased global brain connectivity, allowing different brain regions to communicate in novel ways. Simultaneously, reduced amygdala activity lowers the brain's fear response, creating a window to process difficult emotions safely.
Insights from Preclinical and Animal Studies
Animal studies provide crucial evidence for these effects. For example, research has demonstrated rapid fear extinction in mice, where they unlearn fear responses much faster than normal. An experiment on erasing conditioned fear showed that even low doses of psychedelics could help mice overcome learned fears by promoting new neural connections. These studies consistently show lasting antidepressant effects in rodents and improvements in cognition and social behavior. This research confirms that the benefits of psychedelic therapy reflect real, measurable changes in brain structure and function.
A Guide to Psychedelic Compounds and Their Therapeutic Applications
In psychedelic mental health, different compounds act as unique tools for healing. Each has a distinct mechanism, duration, and therapeutic application, allowing for custom treatments.
Key Psychedelic Compounds
- Psilocybin: The classic psychedelic found in "magic mushrooms." It produces a 4-6 hour introspective journey and shows great promise for depression, end-of-life anxiety, and addiction.
- MDMA: An "empathogen" that increases feelings of trust and emotional openness for 3-6 hours. It is highly effective in therapy for PTSD, as it allows patients to process trauma without being overwhelmed by fear.
- LSD: A long-lasting psychedelic (8-12 hours) with effects similar to psilocybin. It is being studied for anxiety and alcohol use disorders.
- Ketamine: A legal anesthetic used off-label for mental health. It works differently from classic psychedelics, creating a short (45-120 minute) dissociative state with rapid antidepressant effects.
- Ayahuasca & DMT: Ayahuasca is a ceremonial brew containing DMT that produces an intense 4-8 hour journey. DMT alone offers a very short (5-30 minute) but profound visionary experience. Both are being explored for depression and substance use disorders.
Focus on Ketamine
Ketamine holds a special place in psychedelic mental health because it is already a legal, Schedule III substance available for medical use. This makes it the most accessible psychedelic therapy today, allowing patients to receive treatment now rather than waiting for future FDA approvals.
Ketamine's most significant advantage is its speed. It can lift severe, treatment-resistant depression within hours, offering life-saving relief for those with suicidal thoughts. Studies show therapeutic response rates of 50-70% within a day of treatment and a significant decrease in suicidal ideation with repeated sessions.
Its versatility extends to PTSD, bipolar disorder, and chronic pain. The experience is typically dissociative, creating a sense of separation from one's pain and rigid thought patterns, which provides a unique opportunity for new perspectives. By establishing a track record of safety and efficacy under medical supervision, ketamine has paved the way for broader acceptance of other psychedelic therapies.
The Framework of Psychedelic-Assisted Therapy: Safety, Preparation, and Integration
Psychedelic mental health treatment is not a passive experience; it's a structured process called psychedelic-assisted psychotherapy (PAP). The substance is merely a catalyst. True healing comes from the therapeutic framework surrounding it. The core principle is "set and setting"—your mindset (set) and the physical/interpersonal environment (setting) are crucial for a positive outcome.
A strong therapeutic alliance with trained professionals provides an anchor through the three-phase model: preparation, dosing, and integration.
Preparation: Setting the Stage for a Therapeutic Journey
This foundational phase ensures safety and maximizes therapeutic potential. Key steps include:
- Screening: A thorough review of medical and psychological history to ensure candidacy and rule out contraindications (e.g., psychosis, certain heart conditions).
- Building Trust and Setting Intent: Multiple sessions are spent with facilitators to build rapport, establish therapeutic goals, and clarify intentions for the journey.
- Education and Safety: Therapists educate the participant on what to expect, including how to steer challenging moments. This knowledge, combined with clear safety protocols, reduces fear and creates a secure container.
- Managing Expectations: It's vital to understand that psychedelics are tools for healing, not magic bullets. The participant must be prepared to do the work.
The Dosing Session: A Guided Experience
The session occurs in a controlled, comfortable environment. Trained therapists are present throughout, offering a reassuring presence without directing the experience. They provide non-directive support, holding space for whatever arises. The use of music and eye shades helps facilitate an inward journey. Should difficult emotions or potential for paranoia or more severe anxiety emerge, therapists are skilled in navigating these moments, reminding the participant of their safety and the temporary nature of the experience.
Integration: Making Sense of the Experience
Integration is arguably the most critical phase, where insights from the session are translated into lasting change. Without it, a profound experience can fade into a mere memory. Integration involves:
- Post-session psychotherapy: Sessions dedicated to processing the experience, exploring emotions, and examining insights.
- Translating insights into action: Working with a therapist to apply new perspectives to daily life, relationships, and behaviors.
- Supportive practices: Using tools like journaling, mindfulness, and community support groups to solidify and continue the healing process.
The goal of integration is to harness the brain's temporary boost in plasticity to create meaningful, positive changes in one's life.
The Future of Psychedelic Mental Health: Research, Challenges, and Accessibility
The field of psychedelic mental health is on the cusp of a paradigm shift, but significant problems remain before these therapies are widely accessible.
Current Clinical Trials and Future Research
Research is expanding rapidly. Clinical trials are now exploring psychedelics for eating disorders, OCD, substance use, and even Alzheimer's. Exciting new frontiers include the development of non-hallucinogenic "psychoplastogens" that could offer neuroplastic benefits without an intense psychedelic experience, potentially making treatment more scalable. Head-to-head trials comparing psychedelics to standard antidepressants are also underway to establish their efficacy more clearly.
Overcoming Barriers to Access and Affordability
Despite promising research, major challenges must be addressed:
- High Cost: The current therapy model is resource-intensive, with treatments costing thousands of dollars, raising equity concerns.
- Insurance Coverage: As most therapies are not yet FDA-approved, insurance coverage is rare, leaving patients to pay out-of-pocket.
- Therapist Training: A massive effort is needed to train and certify enough therapists to administer these treatments safely and effectively.
- Scalability: The high-touch, one-on-one nature of the therapy makes it difficult to scale to meet the enormous public need.
- Stigma: Lingering stigma from the "War on Drugs" era can hinder public acceptance and policy reform.
Understanding the Long-Term Effects and Potential for Relapse
Long-term data is still being gathered, but initial results are promising, with some studies showing benefits lasting a year or more. Unlike daily medications, psychedelic therapy aims for fundamental, persistent change. However, the potential for relapse underscores the critical importance of ongoing integration and therapeutic support. While classic psychedelics have a low risk of physical dependency, maintaining the benefits often requires continued engagement with the healing process, sometimes including "booster sessions."
Conclusion: A Paradigm Shift in Healing the Mind
We are witnessing a remarkable shift in mental healthcare. Psychedelic mental health offers profound hope for millions struggling with treatment-resistant conditions like PTSD, depression, and anxiety.
Unlike conventional drugs that manage symptoms, psychedelics can help rewire the brain. By promoting neuroplasticity, they break the rigid neural patterns underlying mental suffering. The results are compelling: psilocybin provides sustained relief from depression, MDMA helps the vast majority of PTSD patients no longer meet diagnostic criteria, and ketamine offers rapid, life-saving effects.
Crucially, these substances are catalysts for therapy, not standalone cures. The healing occurs within a structured therapeutic framework that includes meticulous preparation, a guided session, and—most importantly—thorough integration to translate insights into lasting change. This new paradigm moves beyond symptom management to address the root causes of suffering.
While challenges like cost and accessibility remain, the momentum is undeniable. At KAIR Program, we are at the forefront of this change. Our ketamine-assisted retreats merge the rapid benefits of ketamine with intensive, trauma-focused therapy in a supportive setting. Our expert-led team guides participants through the complete journey, from preparation to integration, to ensure lasting healing.
The future of mental healthcare is moving from managing symptoms to facilitating genuine growth. For those ready to explore this new frontier, learn more about our ketamine-assisted retreats and find how we are helping people reclaim their lives through the power of psychedelic mental health treatment.



