Ketamine Therapy: A Lifeline for Treatment-Resistant Depression
When Standard Depression Treatments Fall Short
Ketamine for resistant depression has emerged as a treatment for the millions who haven't found relief through traditional therapies. If you've tried multiple antidepressants, undergone years of psychotherapy, or feel stuck in a cycle of chronic suffering despite your best efforts, you're not alone.
Quick Answer for Ketamine for Resistant Depression:
- What it is: A rapid-acting antidepressant that works on the brain's glutamate system (not serotonin like traditional antidepressants)
- Who it helps: People with treatment-resistant depression who haven't responded to 2+ standard antidepressants
- How fast it works: Relief can begin within 40 minutes to hours (not weeks like SSRIs)
- Success rates: 45-70% response rate and 30% remission rate in real-world studies
- Key benefit: Creates new brain connections and reverses depression-related brain shrinkage
Nearly one-third of the 9 million Americans treated for depression annually have treatment-resistant depression (TRD). This means standard treatments like SSRIs, SNRIs, and psychotherapy haven't provided adequate relief, often leading to feelings of hopelessness and the belief they are "beyond help."
Jeff Winograd's story captures this struggle. He didn't know an adult life without depression and had "tried virtually every antidepressant on the market" since age 20. As he put it, "The depression was just a constant." Then ketamine changed everything, helping him find what he called his "happy place" for the first time in decades.
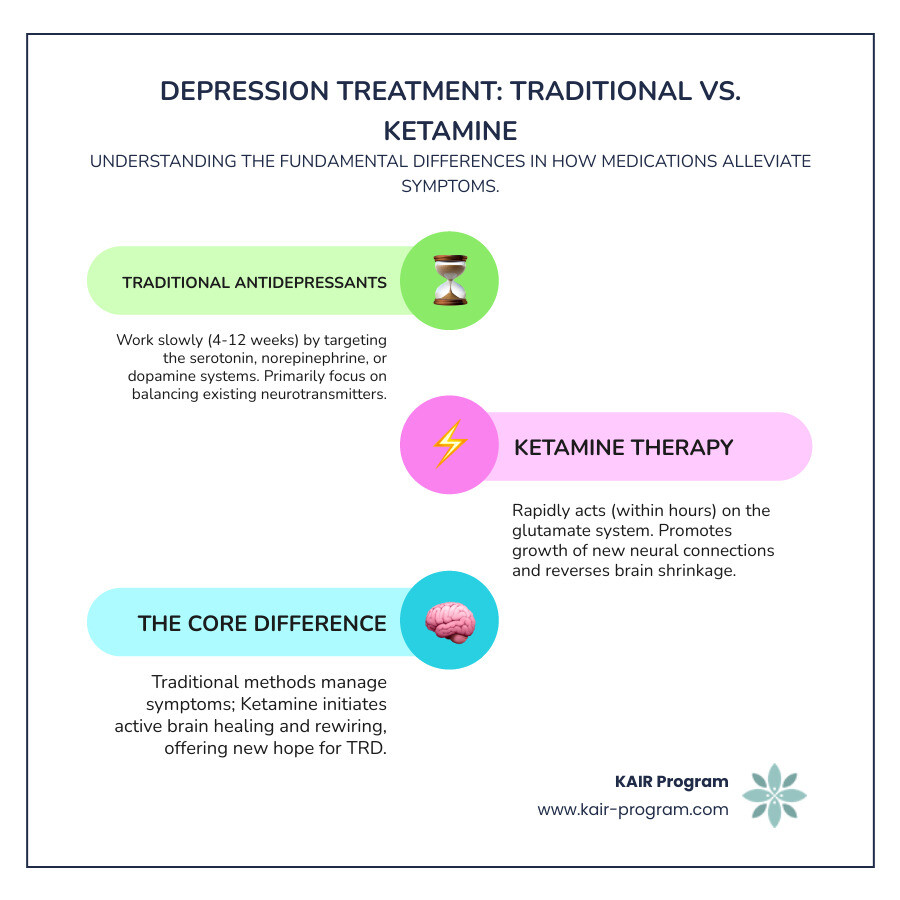
Traditional treatments work slowly on the serotonin system and can take 4-12 weeks to show effects. Ketamine works differently - it rapidly targets the brain's glutamate system, promoting the growth of new neural connections within 24 hours. This isn't just symptom management; it's actual brain healing.
Studies show that people with depression can experience up to 20% shrinkage of the hippocampus, a brain region critical for memory and learning. Within 24 hours of medically supervised ketamine treatment, lost brain connections can start to regrow, offering hope where traditional treatments have failed.
I'm Dr. Bambi Rattner, a licensed psychologist with over 35 years in mental health, specializing in trauma-focused therapies and intensive treatment. Through my work with treatment-resistant patients, I've seen how ketamine for resistant depression creates breakthrough moments when combined with psychotherapy, opening windows of neuroplasticity for deep, lasting healing.
The Science Behind Ketamine for Resistant Depression
For decades, depression treatment focused on a single theory: that depression stems from imbalances in brain chemicals like serotonin, norepinephrine, and dopamine. Traditional antidepressants work by slowly increasing these chemicals over weeks or months. But what happens when this approach doesn't work?
If you've tried multiple SSRIs or SNRIs without success, you know how frustrating this is. It's like trying to fix a complex engine problem by only adjusting the oil levels—the real issue remains untouched.
Ketamine for resistant depression represents a completely different approach. Instead of targeting serotonin, ketamine works on your brain's glutamate system—the most abundant communication network in your central nervous system. This isn't just a new medication; it's a new way of understanding how we can help the brain heal from depression.
When ketamine enters your system, it acts as an NMDA receptor antagonist. Think of NMDA receptors as tiny gates on your brain cells. Ketamine temporarily blocks these gates, which triggers a surge of glutamate throughout your brain.
This glutamate surge activates other important receptors called AMPA receptors, which are crucial for rapid communication between neurons. The result? Your brain releases Brain-Derived Neurotrophic Factor (BDNF)—essentially "miracle grow" for your brain cells.
This process, called synaptogenesis, promotes the rapid growth of new connections between brain cells. Depression causes your brain to shrink, particularly in areas like the hippocampus that are critical for memory and emotional regulation. Ketamine helps reverse this shrinkage by encouraging your brain to build new neural pathways and restore lost connections.
How Ketamine Rewires the Brain for Rapid Relief
Here's where ketamine for resistant depression gets truly remarkable: the speed at which it works. While traditional antidepressants take 4-12 weeks to show effects, ketamine can provide relief within hours—sometimes as quickly as 40 minutes after treatment begins.
This rapid response happens because ketamine isn't just adjusting chemical levels. It's actually repairing and rebuilding the neural pathways that depression has damaged.
Imagine your brain's communication network as a city with roads connecting different neighborhoods. Depression is like a series of earthquakes that have damaged these roads, making it hard for different parts of your brain to communicate. Traditional antidepressants might slowly patch a few potholes, but ketamine acts like a rapid reconstruction crew, clearing debris and building new, stronger roadways.
This rapid neuroplasticity means that lost brain connections can start to regrow within just 24 hours of your first medically supervised ketamine treatment. Scientific research on ketamine-stimulated synaptogenesis shows how this process literally helps your brain heal itself at the cellular level.
This is a fundamental shift from traditional treatments. Instead of just managing symptoms by adjusting neurotransmitter levels, we can now promote actual healing and restore brain function.
Ketamine Treatment Modalities: What Does KAIR Offer?
When exploring ketamine for resistant depression, it's important to understand that not all ketamine treatments are the same. Ketamine has been safely used as an anesthetic for over 50 years, but for depression treatment, we use much lower, "sub-anesthetic" doses that allow you to remain conscious and aware.
At KAIR, we focus on IV ketamine infusions and oral/compounded ketamine options like lozenges or troches. Each method has distinct advantages depending on your needs and treatment goals.
IV infusions offer the most precise dosing and rapid onset, making them ideal for initial treatment phases. The medication goes directly into your bloodstream, ensuring consistent bioavailability and allowing for careful monitoring.
Oral forms provide more flexibility and can be useful for maintenance treatments or as part of ongoing therapy protocols. These compounded medications are prepared specifically for therapeutic use under strict medical supervision.
Our approach at KAIR integrates these ketamine modalities into a comprehensive treatment that combines ketamine's neuroplasticity benefits with intensive, trauma-focused therapy. This integration sets our program apart; we use ketamine as a catalyst for deeper therapeutic work and lasting healing.
You can learn more about how we tailor these different approaches to each individual's needs through the KAIR Program's approach to ketamine therapy.
The Ketamine Treatment Journey: What to Expect
Taking the first step toward ketamine for resistant depression can feel both hopeful and nerve-wracking. You might wonder: What will it feel like? Is it safe? Is it right for me?
Let me walk you through a typical ketamine treatment journey, so you know what to expect.

Safety always comes first. Ketamine must be administered under strict medical supervision in certified clinical settings. This isn't something you should try on your own—the therapeutic benefits come from the careful balance of proper dosing, medical oversight, and professional support.
The concept of "set and setting" is crucial. Your mindset going into treatment (the "set") and the physical environment (the "setting") directly impact your experience. That's why reputable clinics create calm, supportive spaces that feel more like a cozy living room than a sterile medical facility.
Your journey begins with a thorough consultation. Our medical team will review your mental health history, medications, and overall health to determine if ketamine is right for you. We'll also discuss your goals and any concerns. This isn't a one-size-fits-all treatment—everything is customized to your needs.
During the treatment session, you'll be in a comfortable reclining chair, with healthcare professionals monitoring you throughout. Many people describe entering a dissociative state—feeling disconnected from their body or surroundings. This might sound scary, but it's a normal part of how ketamine works its magic on your brain.
The experience varies. Some describe it as floating or dreaming while awake; others feel like they're observing their thoughts from a distance. These effects last for the duration of the treatment and fade as the session ends.
The recovery period is just as important as the treatment itself. You'll be observed as the immediate effects wear off, and many people find this a peaceful time for reflection. This flows into what we consider the most crucial part: post-treatment integration.
Methods of Administration and Their Implications
When considering ketamine for resistant depression, the way it's delivered makes a significant difference in your experience and results.
IV ketamine infusions are administered directly into your bloodstream. This method offers 100% bioavailability—meaning all of the medicine reaches your system. The effects begin within minutes, and your medical team can adjust the dose in real-time. These sessions typically last about 40 minutes, with the dissociative experience fading 15-20 minutes after the infusion ends. The entire experience, from start to complete recovery, usually takes about 2 hours.
Oral or compounded ketamine comes in forms like lozenges or troches that dissolve under your tongue. While more convenient, these have much lower bioavailability—typically only 17-20% of the medicine reaches your bloodstream due to how your liver processes it. This means you need a higher dose to achieve similar effects to IV treatment. The onset is also slower, taking 15-45 minutes to feel the effects.
| Feature | IV Ketamine (Intravenous Infusion) | Oral/Compounded Ketamine (Lozenges, Troches) |
|---|---|---|
| Administration Setting | Clinic/Medical Office, under direct medical supervision | Can be prescribed for at-home use, but initial doses often in clinic, with ongoing supervision |
| Bioavailability | 100% (directly into bloodstream) | Variable, typically 17-20% (due to first-pass metabolism in the liver) |
| Typical Cost Structure | Per infusion, often higher upfront costs | Per prescription, generally lower per dose than IV |
A word of caution: The FDA has issued important warnings about compounded ketamine products, especially those from mail-order services. The FDA warning about risks of compounded ketamine products emphasizes why medical supervision is so critical for your safety.
The Critical Role of Therapeutic Integration
Here's where the real magic happens, and it's not just the ketamine.
Ketamine acts as a powerful catalyst for change, but it's not a cure-all. Think of it as opening a window in your mind that's usually locked shut. During this window of improved neuroplasticity, your brain becomes more flexible and open to new ways of thinking and processing emotions.
Without proper therapeutic support, this window might close without lasting change. That's why we believe combining ketamine with expert psychotherapy isn't just helpful—it's essential for real, lasting healing.
The dissociative experience during ketamine treatment can bring up profound insights, buried memories, or intense emotions. You might gain new perspectives on old problems or feel emotions you've avoided for years. A skilled therapist helps you make sense of these experiences and translate them into practical changes in your daily life.
Our approach emphasizes trauma-focused therapy and evidence-based methods like Cognitive Behavioral Therapy (CBT). During your improved neuroplasticity period, these therapeutic techniques become more powerful. It's like having a skilled guide while exploring new territory in your mind.
As renowned psychiatrist John Krystal, MD, explains: "The ketamine treatment is the reaction of your brain to ketamine, how your brain responds to exposure to ketamine." But he's quick to add that "the notion of 'treatment' is much broader than that."
This broader treatment includes the crucial work of therapy—helping you process insights, develop healthier coping strategies, and reshape your brain for lasting wellness. This comprehensive approach is at the heart of what we do, and you can find more info about our integrated treatment approach.
Efficacy, Safety, and Patient Suitability
When considering ketamine for resistant depression, it's natural to want clear answers about its efficacy, risks, and if you're a good candidate. After years of failed treatments, hope can feel fragile. Let's review what the research shows so you can make an informed decision for your healing journey.
This isn't a decision you'll make alone. The best outcomes happen when you work closely with experienced medical professionals who understand both the benefits and risks. It's a collaborative process between you and your healthcare provider.
Demonstrated Efficacy of Ketamine for Resistant Depression
The evidence supporting ketamine for resistant depression is compelling, offering real hope for those who have found little relief. Research shows:
- High Response Rates: 45-70% of patients with TRD show significant improvement. In clinical trials with IV ketamine, response rates have reached as high as 70%.
- Significant Remission Rates: About 30% of people achieve remission, where depressive symptoms reduce dramatically or disappear entirely.
- Rapid Symptom Reduction: Relief can begin within 40 minutes, a stark contrast to the weeks or months required for traditional antidepressants.
- Powerful Anti-Suicidal Effects: Ketamine can reduce suicidal thoughts within hours, making it a critical tool for crisis intervention.
- Sustained Improvement: Research shows promising long-term results, with many people maintaining their improvement for weeks or months with maintenance treatments.
These statistics represent real people who had given up hope, then found their way back to life. Ketamine for resistant depression provides much-needed hope for individuals who have endured the frustrating cycle of failed treatments.
Who is a Candidate for Ketamine for Resistant Depression?
Ketamine for resistant depression isn't for everyone, and the careful screening process helps ensure you get the treatment that's most likely to help you.
You're typically a candidate if you have a confirmed diagnosis of treatment-resistant depression (TRD). This means you've tried at least two different antidepressant medications for adequate time periods—usually 6-8 weeks each at appropriate doses—without getting the relief you need.
Severe Major Depressive Disorder is the primary condition we treat, though ketamine has also shown promise for bipolar depression in specific research contexts. If you're dealing with depression with suicidal ideation, ketamine's rapid anti-suicidal effects can be life-saving.
The key is having exhausted other options first. We're not talking about someone who tried one antidepressant for a few weeks. We're talking about people who have genuinely tried multiple approaches over months or years without adequate improvement.
Before starting treatment, you'll go through comprehensive medical and psychiatric screening. This includes reviewing your complete medical history, current medications, and a thorough psychological assessment to ensure ketamine is both safe and appropriate for you.
Potential Side Effects, Risks, and Contraindications
Like any powerful medicine, ketamine comes with potential side effects and risks. The difference is that we monitor everything carefully and discuss all possibilities beforehand.
Short-term side effects happen during and immediately after treatment, but they're temporary and resolve within a few hours. The most common is dissociation—that "out-of-body" feeling or sense of detachment. This often peaks around 40 minutes into treatment and wears off within two hours. While it can feel strange, it's an expected part of the healing process.
Nausea can occur, but we can manage it with anti-nausea medication. Your blood pressure and heart rate may increase temporarily, which is why we monitor your vital signs closely. Some people experience dizziness, headaches, or blurred vision, and occasionally temporary anxiety during the dissociative phase.
Long-term risks are primarily associated with unsupervised or recreational use, not medical treatment. While ketamine is a Schedule III drug with potential for misuse, the risk is very low when administered in controlled medical settings. Chronic, high-dose recreational use can cause severe bladder problems, but this is extremely rare with medically supervised treatment.
There are important contraindications where ketamine treatment is generally avoided. Active psychosis or a history of schizophrenia makes ketamine unsuitable. Uncontrolled high blood pressure (over 160/90) is problematic because ketamine can raise it. Severe heart conditions, active substance abuse, pregnancy or breastfeeding, and current delirium or dementia are also typically contraindications.
Our medical team conducts a thorough assessment to determine if ketamine therapy is right for you. Your safety always comes first, and we'll only proceed if we believe the benefits clearly outweigh any risks.
Practical Considerations: Cost and Insurance Coverage
Let's discuss the financial side of ketamine for resistant depression treatment. Understanding the costs is essential for planning your path to healing.
Investing in your mental health, especially with innovative treatments like ketamine, requires financial planning. However, for those who have struggled for years with TRD, the cost of continuing to suffer—in lost productivity, relationships, and quality of life—often far exceeds the investment in effective treatment.
How Much Does Ketamine Therapy Cost?
The cost of ketamine for resistant depression varies based on how it's given and where you receive treatment.
IV ketamine infusions typically run around $600 per session. Most people need an initial series of six infusions over two to three weeks for optimal results. This means you're looking at roughly $3,600 for your initial treatment course.
After that initial series, many patients need maintenance sessions every few weeks or months. The frequency depends on your individual response and how long the benefits last.
Oral or compounded ketamine (the lozenges or troches) generally costs less per dose than IV treatments. Since these are take-home medications, you're not paying for clinic time and medical supervision with each dose. However, the total cost depends on how often you need to take them.
Several factors influence your overall investment: the number of treatments you need, whether you're combining ketamine with psychotherapy (which we strongly recommend), and the specific services your clinic provides. At KAIR, our integrated approach means you're getting comprehensive care, not just the medication.
Is Ketamine Treatment Covered by Insurance?
This is where things get complicated. Most forms of ketamine for resistant depression are considered "off-label," meaning insurance companies typically don't cover them directly.
IV ketamine and oral compounded ketamine fall into this category. While ketamine is FDA-approved as an anesthetic, its use for depression is off-label. This means most patients pay out-of-pocket for these treatments.
But don't lose hope. Some clinics can provide you with a "superbill"—a detailed receipt of your medical services. You can submit this to your insurance company for potential reimbursement as an out-of-network provider. Whether they'll reimburse you depends entirely on your specific plan.
Here's a helpful tip: Health Savings Accounts (HSA) and Flexible Spending Accounts (FSA) often cover ketamine treatments. Since these accounts use pre-tax dollars for healthcare expenses, they can significantly reduce your out-of-pocket costs.
The financial aspect shouldn't be the only factor, but it's worth discussing with our team. We understand that cost is a real consideration, and we're here to help you understand all your options to get you the care you need.
Conclusion: A New Chapter in Mental Health Treatment
The emergence of ketamine for resistant depression has fundamentally changed how we treat severe mental health conditions. For decades, people with TRD felt trapped in cycles of failed treatments, believing they were "unfixable." Ketamine has rewritten that story.
This isn't just another antidepressant. We're talking about a complete paradigm shift from slow symptom management to rapid brain healing. Traditional treatments try to adjust chemical levels over weeks or months. Ketamine actually rebuilds the neural pathways that depression has damaged, often within hours of the first treatment.
The numbers speak for themselves—response rates of 45-70% in people who haven't responded to anything else. But beyond statistics, ketamine offers something more precious: hope restored. When someone has tried multiple medications and years of therapy without success, ketamine can be the breakthrough that changes everything.
The real magic happens when ketamine meets expert therapy. The medicine creates a window of neuroplasticity—a time when your brain becomes more flexible and open to change. This is when skilled, trauma-focused therapy can do its deepest work. It's like a master gardener tending to soil that's suddenly become fertile again.
Research continues to expand ketamine's potential beyond depression. Scientists are exploring its effects on PTSD, OCD, chronic pain, and addiction. Each study reveals new possibilities for conditions that have been difficult to treat. Insights from ketamine research are also inspiring next-generation treatments that could help even more people.
At KAIR, we've built our approach around maximizing ketamine's healing potential. Our integrated model combines the neuroscience of ketamine with intensive, expert-led therapy. We don't just give you the medicine; we create a comprehensive healing environment where the neuroplasticity ketamine provides can be channeled into lasting, transformative change.
If you've been struggling with treatment-resistant depression and feel like you've exhausted your options, ketamine therapy might be the new chapter you've been waiting for. The combination of rapid neurological healing and intensive therapeutic work can create profound shifts that seemed impossible before.
This is more than another treatment option; it's a fundamental shift toward healing that addresses both the biology and psychology of depression. When medicine and therapy work together, the results can be transformative.
Ready to explore what this new chapter could look like for you? Learn more about our Ketamine-Assisted Intensive Retreats and find how our integrated approach can help you find the lasting recovery you deserve.
