Trauma Recovery Therapies That Actually Make a Difference
Why Understanding Your Treatment Options Matters for Lasting Recovery

Therapy for trauma recovery offers hope and healing for the millions of people who carry the invisible wounds of difficult experiences. Whether you're dealing with a single traumatic event or complex, long-term trauma, the right therapeutic approach can make all the difference in reclaiming your life.
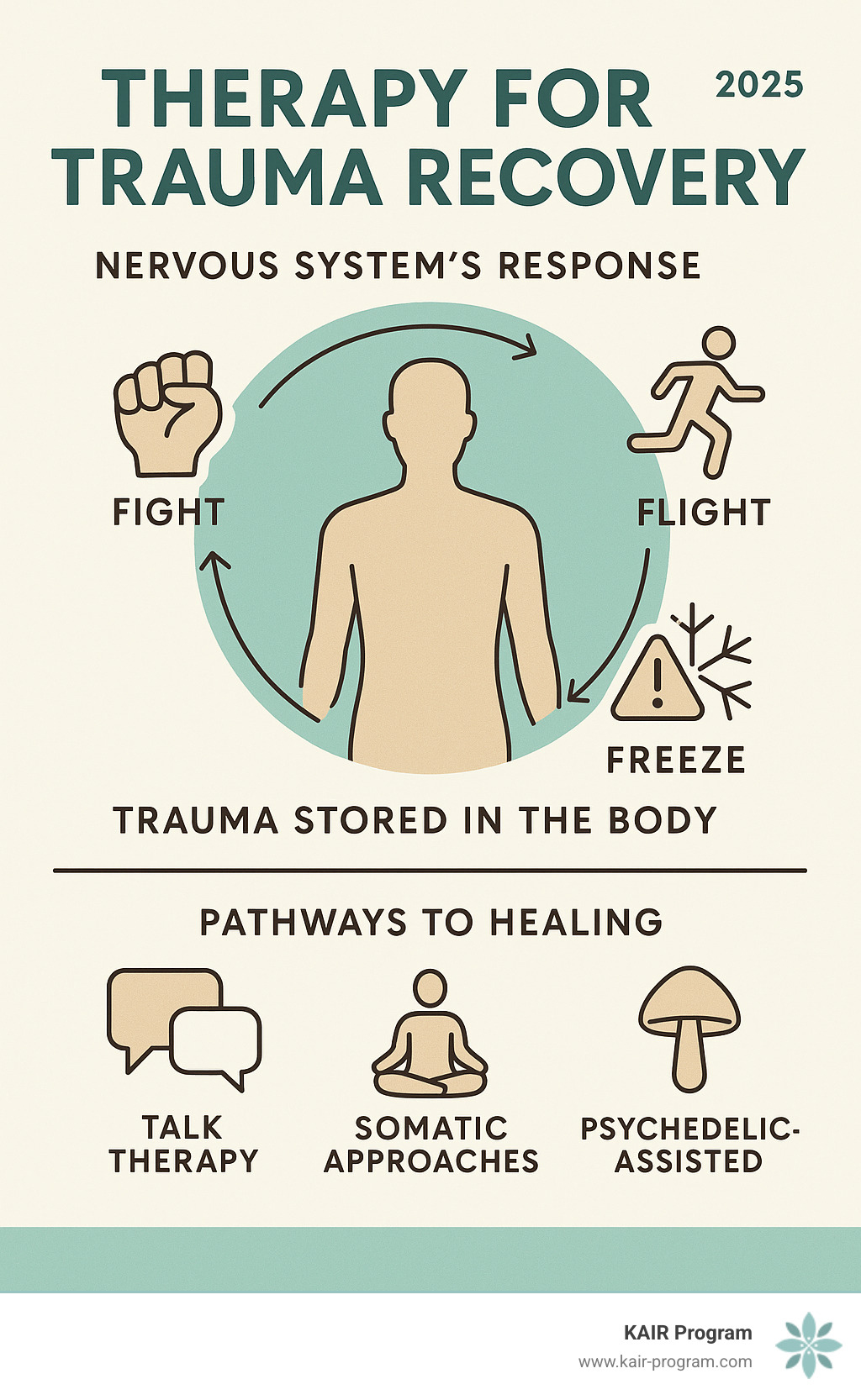
Evidence-based trauma therapies that actually work include cognitive approaches like CPT, exposure-based methods like PE, and mind-body modalities like EMDR and Somatic Experiencing. Around 70% of adults in the United States have experienced at least one trauma, yet only 6% develop PTSD. This shows that while trauma is common, with the right support, recovery is absolutely possible.
Trauma doesn't just affect your mind—it changes your brain and nervous system. You might experience hypervigilance, emotional numbness, or flashbacks. These aren't character flaws; they're normal responses to abnormal experiences.
The good news? Modern trauma therapy has evolved far beyond just "talking about it." Today's approaches work with both your mind and body to create lasting change, with some people seeing significant improvement in weeks rather than years.
As Bambi Rattner, PsyD, I've spent decades working with trauma survivors and have seen how the right therapy for trauma recovery can transform lives. My experience with EMDR, intensive therapy models, and trauma retreats has shown me that healing is not only possible—it can happen faster than most people think.
Understanding Trauma's Impact and the Need for Professional Care
The statistics around trauma are staggering. Around 70% of adults in the United States have experienced at least one trauma, which means if you're reading this, you're not alone.
Trauma is defined as exposure to actual or threatened death, serious injury, or sexual violence. This can be experienced directly, witnessed, or learned about happening to a loved one. First responders often experience trauma through repeated exposure to distressing situations.
What makes trauma so complex is how it literally changes your brain and body. Your nervous system can get stuck in survival mode, creating what we call nervous system dysregulation. You might feel constantly on high alert or, conversely, completely numb and disconnected.
Emotionally, this can lead to persistent sadness, anxiety, or wild mood swings. Physically, trauma often shows up as chronic pain, exhaustion, digestive issues, or a constant jumpy feeling. These are real physical responses to what you've been through.
This is why self-help isn't always enough. While practices like mindfulness and exercise are helpful, trauma memories are often stored in parts of the brain that talk therapy alone can't reach. They can affect you in ways you might not even realize.
Professional therapy for trauma recovery is essential. A skilled trauma therapist creates a safe space and uses specific tools to help you process what happened and how it's affected you. The sooner you access good treatment, the sooner you can start feeling like yourself again.
What is Trauma-Informed Care?
The most important shift in trauma treatment has been moving from "What's wrong with you?" to "What happened to you?" This change sees your symptoms not as problems to fix, but as normal responses to abnormal experiences.
Trauma-informed care is built on several core principles:
- Safety: Creating a space where you feel physically, emotionally, and psychologically secure.
- Trustworthiness: Ensuring the therapist is consistent, reliable, and transparent.
- Collaboration: Recognizing you are the expert on your own experience and working with you.
- Empowerment: Helping you reclaim your sense of agency, strength, and control.
This approach is guided by the '4 R's' of trauma-informed care: Realizing the widespread impact of trauma, Recognizing its signs and symptoms, Responding by integrating this knowledge into all practices, and actively working to Resist re-traumatization.
This framework changes everything. A trauma-informed therapist understands that certain behaviors are protective, not difficult. The question "What happened to you?" opens the door to understanding and compassion, which is the foundation for effective and sustainable healing.
Foundational Evidence-Based Psychotherapies for Trauma
When you're ready to heal from trauma, it helps to know which treatments are proven to be effective. Therapy for trauma recovery now includes structured, evidence-based practices that create real, lasting change by addressing the root causes of your distress.
The American Psychological Association recommends treatments that focus on cognitive restructuring (challenging unhelpful thoughts) and emotional processing (working through difficult feelings and memories safely). These approaches help your brain integrate traumatic experiences so they no longer control your life.

Cognitive Behavioral Therapy (CBT) and Its Variations
CBT works on the principle that your thoughts, feelings, and behaviors are connected. By changing one, you can influence the others. Trauma-Focused CBT adapts this for trauma survivors, helping you identify false beliefs, develop healthy coping skills, and express emotions safely over 12 to 20 sessions.
Cognitive Processing Therapy (CPT) specifically targets how trauma changes your beliefs. It helps you challenge "stuck points"—thoughts like "I should have known" or "The world is completely dangerous." In about 12 sessions, CPT addresses key areas impacted by trauma: safety, trust, power, self-esteem, and intimacy, leading to significant, lasting improvements in PTSD symptoms.
Prolonged Exposure (PE) helps you reclaim your power by gradually and safely facing trauma-related memories and situations you've been avoiding. This happens through imaginal exposure (describing the trauma in detail) and in-vivo exposure (confronting real-world situations). PE typically takes 8 to 15 sessions and teaches your brain that these reminders are no longer dangerous.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a highly effective trauma therapy that changes how traumatic memories are stored in your brain. Developed by Francine Shapiro, EMDR helps your brain's natural healing process kick in, allowing it to properly "digest" memories that have become "stuck."
EMDR uses bilateral stimulation—usually guided eye movements, but sometimes alternating sounds or taps—while you briefly focus on a traumatic memory. This stimulation helps desensitize you to the memory's emotional charge.
EMDR follows 8 structured phases, from preparation to processing and re-evaluation. A complete course for complex trauma typically takes 6 to 12 sessions. The results are well-documented; a Kaiser Permanente study found that 100% of single-trauma survivors and 77% of those with complex trauma benefited from EMDR. For those seeking faster results, EMDR Therapy Intensives offer concentrated treatment in a retreat-like setting.
Exploring Somatic and Integrative Trauma Therapies
We now know that trauma doesn't just live in our heads; it gets stored in our bodies and nervous systems. This mind-body connection is why talking alone is sometimes not enough for complete trauma healing. Releasing stored trauma often requires "bottom-up processing," starting with bodily sensations to understand and heal.
As Dr. Peter Levine, developer of Somatic Experiencing, noted, the body holds the key to open uping frozen trauma responses. Your nervous system wants to heal; it sometimes just needs the right guidance.
Somatic Therapies: Healing the Body's Memory
Somatic therapies work directly with how trauma shows up in your body, helping to regulate a nervous system that may be stuck in hyperarousal or numbness.
Somatic Experiencing (SE) helps you complete the fight, flight, or freeze responses that got stuck in your system. Through body awareness, you learn to notice physical sensations and help your nervous system finish what it started. This is done through titration (processing small, manageable bits of trauma) and pendulation (gently moving between states of tension and calm) to build resilience. Practices that promote vagus nerve stimulation, like deep breathing, humming, or cold showers, are also key to calming the nervous system, a concept highlighted in The Body Keeps the Score.
Internal Family Systems (IFS) and Other Relational Models
Powerful healing also comes from exploring our inner world and relationships.
Internal Family Systems (IFS) views the mind as having different "parts." After trauma, protector parts (like anxiety or anger) emerge to keep you safe, while exiled parts hold the pain and shame. The goal is to connect with your Core Self—the wise, compassionate center within—to lead and heal these parts.
Other integrative models offer unique paths to healing. Narrative Therapy helps you rewrite the dominant, often negative, story that trauma created. Inner Child Work involves connecting with and caring for the younger parts of you that were hurt. Art and Music Therapy provide non-verbal outlets to process what words cannot express. Combining these approaches can create a comprehensive path to wholeness.
Advanced and Intensive Options for Deeper Healing
Sometimes, weekly therapy isn't enough, especially for treatment-resistant conditions or for those who want to accelerate their healing. Advanced and intensive options concentrate the therapeutic work into shorter, more focused periods, creating powerful momentum for change.
This focused intensity is often necessary for deep emotional healing. By immersing yourself in the healing process without the week-long gaps of traditional therapy, you can break through long-standing barriers. These advanced trauma treatment methods allow for deeper work to unfold more naturally and quickly.
Accelerated and Intensive Therapy for Trauma Recovery
Accelerated Resolution Therapy (ART) is an exciting development in rapid trauma healing. It helps your brain "reprogram" how it stores traumatic memories, often providing significant relief in just one to three sessions by replacing disturbing images with more peaceful ones.
Intensive trauma therapy condenses treatment into a shorter timeframe, such as working with a therapist for several hours a day over a few days or weeks. Intensive therapy retreats provide an even more supportive environment for this work. By stepping away from daily life, these adult trauma healing retreats create a safe space to process trauma efficiently and thoroughly.
Psychedelic-Assisted Therapy: A New Frontier in Trauma Recovery
Psychedelic-assisted therapy is revolutionizing therapy for trauma recovery, especially for those who haven't found relief with other methods. Healing trauma with psychedelics combines carefully administered psychedelic compounds with expert psychotherapy in a controlled setting.
These substances can temporarily lower psychological defenses and improve neuroplasticity—your brain's ability to form new connections. This creates a unique window of opportunity for processing difficult memories and gaining new insights.
Ketamine-Assisted Psychotherapy (KAP) is at the forefront of this revolution. At KAIR, we specialize in integrating ketamine with trauma-focused therapy. Ketamine therapy for PTSD is particularly effective because it can create an "awakened mind," temporarily freeing you from rigid thought patterns and allowing for profound healing.
Our psychedelic-assisted therapy retreat model provides a comprehensive, supportive environment where this powerful work can unfold safely, creating rapid and lasting change.
What to Expect and How to Support Your Healing Journey
Starting therapy for trauma recovery is a courageous decision. It's natural to feel nervous, but understanding the process can ease your concerns. The journey isn't always linear, but the potential for change makes it worthwhile.
The Benefits and Outcomes of Committing to Therapy
Committing to therapy brings benefits that ripple through every area of your life. The first change is often symptom reduction, as flashbacks, anxiety, and sleepless nights begin to fade. Research shows that up to 80% of people who complete treatment experience significant, lasting improvements in PTSD symptoms.
Your relationships will likely transform as trust rebuilds and connection becomes easier. Your sense of self-worth grows stronger, replacing critical inner voices with self-compassion. You'll also experience nervous system regulation, as your body learns to relax and respond to stress in healthier ways. The ultimate goal is reclaiming your life from the grip of the past.
Finding the Right Therapist and Supporting Your Own Healing
Finding the right therapist is key. Look for someone with specific training in trauma-focused approaches and schedule consultations to find a good fit. The therapeutic alliance—your sense of trust and connection with your therapist—is crucial for healing.
While professional support is essential, you also play a huge role. Self-care practices are medicine for your nervous system. Simple habits like mindfulness, gentle exercise, and good nutrition support your brain's healing process. Support groups can also be incredibly validating, reminding you that you are not alone.
Healing isn't a straight line; be patient with yourself. The most important thing is taking that first step and deciding you deserve to feel better.
Frequently Asked Questions about Therapy for Trauma Recovery
Starting therapy for trauma recovery can bring up many questions. Here are answers to some of the most common concerns.
How long does trauma therapy take?
There's no one-size-fits-all timeline, as your healing journey is unique. However, research provides some general guidelines. Cognitive Processing Therapy (CPT) is typically about 12 sessions, while Prolonged Exposure (PE) often involves 8 to 15 sessions. EMDR therapy usually ranges from 6 to 12 sessions.
Newer approaches can work even faster. Accelerated Resolution Therapy (ART) may bring relief in just one to three sessions. Intensive therapy retreats, like those offered at KAIR, can condense months of weekly therapy into a much shorter, immersive experience. Healing isn't a race; the right pace is the one that works for you.
Will talking about trauma in therapy make my symptoms worse?
This is a valid fear. It's true that some people experience a temporary increase in symptoms when they begin processing trauma. This doesn't mean therapy is making you worse; it's often a sign that the healing process is beginning.
A skilled, trauma-informed therapist knows how to manage this. They prioritize creating safety and building your coping skills before addressing difficult memories. We process trauma gradually at a pace that feels manageable. Think of it like physical therapy for an injury—some initial discomfort can lead to long-term strength and mobility. The long-term relief and freedom are worth the initial challenges.
What is the difference between trauma and PTSD?
This is an important distinction. Trauma is the event itself—the accident, the abuse, the loss. PTSD (Post-Traumatic Stress Disorder) is a specific clinical diagnosis describing a particular set of reactions to that event.
Not everyone who experiences trauma develops PTSD. While around 70% of U.S. adults have experienced a trauma, only about 6% develop PTSD. This highlights human resilience and that healing is the norm, not the exception.
PTSD symptoms fall into four main categories: re-experiencing (flashbacks, nightmares), avoidance of reminders, negative changes in thoughts and mood, and changes in arousal and reactivity (being jumpy, sleep problems). If these symptoms persist for over a month and disrupt your life, you may have PTSD. However, anyone whose life is impacted by trauma can benefit from therapy for trauma recovery.
Take the Next Step on Your Path to Recovery
This guide has shown that healing is possible. From foundational therapies like Cognitive Processing Therapy and EMDR to somatic approaches and innovative Ketamine-Assisted Psychotherapy, there are many effective paths to recovery.
Some find healing through weekly therapy, while others achieve rapid change in intensive retreats. What matters is finding the approach that resonates with your unique needs. You are not limited to one method; combining modalities is often the most effective strategy.
At KAIR Program, we specialize in advanced and intensive options for those who have not found relief through traditional therapy. We integrate cutting-edge treatments like ketamine-assisted therapy with proven trauma-focused approaches in an intensive retreat setting, creating a dedicated space for profound healing.
Taking the first step is often the hardest part. Whether it's scheduling a consultation or simply acknowledging you deserve to feel better, that step takes tremendous courage. You don't have to figure this out alone. Professional guidance can help you steer your options and find the right path.
The path forward is waiting. You've already shown incredible strength by learning about your options—now it's time to take that next brave step toward the life you deserve.


